Avicenna J Environ Health Eng. 10(1):65-71.
doi: 10.34172/ajehe.2023.5381
Review Article
Medical Waste Increase During COVID-19 Pandemic in Asia: A Meta-analysis
Nematollah Jafarzadeh 1, 2  , Heydar Maleki 3, *
, Heydar Maleki 3, * 
Author information:
1Environmental Technologies Research Center (ETRC), Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
2Department of Environmental Health Engineering, School of Health, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
3Department of Environmental Health Engineering, School of Health, Student Research Committee, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
Abstract
The coronavirus disease 2019 (COVID-19) prevalence increased hospital admissions and caused a higher rate of medical waste. In this study, the status of medical wastes and recommended disinfecting methods were reviewed before and during the COVID-19 pandemic in Asia. The published papers, library searching, and website browsing with no language restrictions were used to conduct this analytical-descriptive study before the pandemic until the early months of 2020. The results showed that generation rates of medical waste (GRMW), including surgical gloves, face masks, and the like increased by 10%, 12%, 23%, 28%, 97%, 425, and 1262% in Iran, Tehran, China, Malaysia, Dhaka, Wuhan, and King Abdullah University Hospital, respectively, in 2020 regarding the normal period without any pandemic. The capital or the most engaged city in each country produced higher GRMW compared with the whole country so that the GRMW in Iran, Bangladesh, and China were 13.2%, 29.2%, and 70.4% lower than that in Tehran, Dhaka, and Wuhan, respectively. The GRMW also indicated reverse trends with the number of hospital beds, population, and accumulated confirmed cases.
Keywords: COVID-19, Medical waste, Generation rate, Waste management, Disinfecting methods,
Copyright and License Information
© 2023 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Please cite this article as follows: Jafarzadeh N, Maleki H. Medical waste increase during COVID-19 pandemic in asia: a metaanalysis.Avicenna J Environ Health Eng. 2023; 10(1):65-71. doi:10.34172/ajehe.2023.5381
1. Introduction
The fundamental concerns of the recent decades are waste management and associated health and environmental outcomes. Medical wastes that coincided with the development of science and technology became one of the most important environmental challenges, especially in developing countries (1). Medical wastes include domestic, infectious, pathological, sharp, pharmaceutical, chemical, and radioactive wastes. For the first time, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was released in Wuhan, China, and became a major concern worldwide a few months later (2). The infected person often exhibits symptoms similar to a cold (3,4). Compliance with healthcare principles (e.g., hand washing, social distancing, wearing face masks, and the like) and waste management decreased the spread of the virus especially in schools, supermarkets, meat processing plants, and hospitals (5,6). SARS-CoV-2 survived several hours on different surfaces; for example, it survives 4 hours on copper, 6 hours on stainless steel, and 3 hours on plastic (4,7,8). Another study showed that this virus can survive even to 9 days on plastic, glass, and metal objects (7). The virus often infects people by transferring from high-touch surfaces and coughing. Since the tools used for the treatment of infected people may transfer the active SARS-CoV-2, they are considered infectious wastes. The rise in the amount of infectious and medical wastes caused extra concerns about their management (9). These wastes could have critical consequences on health and the environment.
Extra amounts of personal protective equipment (i.e., gloves, gowns, shoe covers, head covers, masks, respirators, eye protection, face shields, and goggles) became infectious wastes when SARS-CoV-2 prevailed worldwide. These kinds of wastes could also dominate viral diseases in society (10). To say the least, the amount of medical waste increased dramatically during the pandemic; however, the incomplete management of these wastes redoubled environmental and public health concerns (10). Improper collection, disinfecting, transportation, or disposal of medical wastes are the most influential and common phases that cause considerable environmental and health issues, especially during the coronavirus disease 2019 (COVID-19) period (11). In addition to the inappropriate management of solid wastes, the weak design of solid waste containers is one of the reasons that increased the contamination of solid wastes, especially in Asia. The lack of sufficient resources also negatively affected the management of wastes, particularly in countries where open dumping is the most frequent strategy for the management of solid wastes (12,13).
Numerous studies investigated COVID-19-related health and environmental issues as well as the amount of produced medical waste based on many assumptions (e.g., population, COVID-19 cases, urban population portion, and daily rate of facemask use) which led to a considerable amount of medical waste. However, this study aimed to eliminate these assumptions and analyze the amount of the real produced medical wastes before and during the coronavirus pandemic in Asia. The data were collected from responsible organizations or reported in research papers. Different technologies were also evaluated to present the most applicable method for disinfection of medical wastes.
2. Materials and Methods
2.1. Study Design
All published reports and papers, mostly until 2020, that evaluated the relationship between COVID-19 incidences and medical wastes were gathered and reviewed to present the status of medical wastes before and during the COVID-19 pandemic. The same process was used for the evaluation of recommended disinfecting devices. Due to the irregular situation at the beginning of the pandemic, the generation rate of medical waste was at the highest amount; therefore, the early months of 2020 were considered in this study. Information was obtained from Web of Science, Scopus, PubMed, Google Scholar, The World Health Organization (WHO), and relevant websites. In the first step, the following items were searched to find appropriate documents: Waste, medical wastes, waste management, hospital wastes, clinical wastes, COVID-19 exposure, COVID-19 transmission, COVID-19 cases and deaths, autoclave, microwave, chemical disinfecting, landfilling, incinerators, China, India, Bangladesh, Australia, and Malaysia. In the current study, the total number of documents included 39 references of which 30 references were used and analyzed in the results and discussion section (Fig. 1). The results and discussion of the study were evaluated in two sections: (a) The generation rate of medical waste before and during the COVID-19 pandemic and (b) Disinfecting methods of medical wastes during the COVID-19 pandemic.
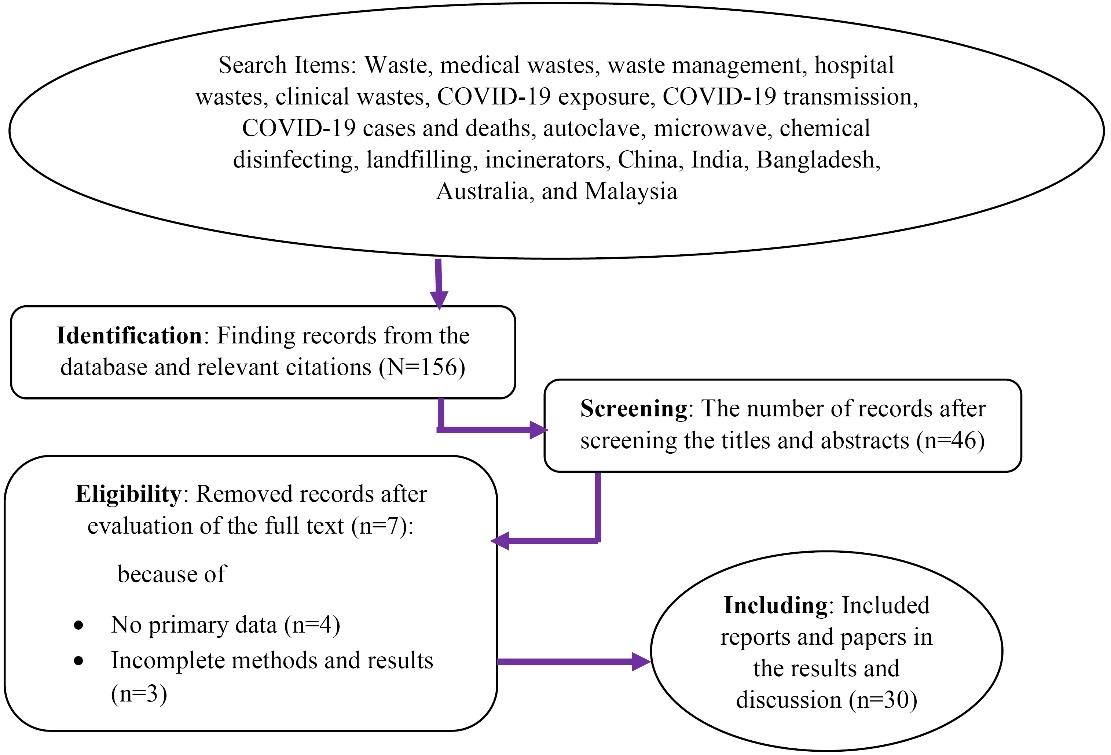
Fig. 1.
Searched Items, Screened and Included Papers, Evaluating GRMW by Preferred Reporting Items for Systematic Reviews and Meta-analysis in the Current Study. Note. GRMW: Generation rates of medical waste
.
Searched Items, Screened and Included Papers, Evaluating GRMW by Preferred Reporting Items for Systematic Reviews and Meta-analysis in the Current Study. Note. GRMW: Generation rates of medical waste
No language limitation was imposed in the current study. This study was conducted based on the available information, including population, the generation rate of medical waste, hospital beds, and the number of patients in Asia. One of the limitations of this study was the lack of available statistics on the number of confirmed coronavirus cases per city in most countries. Furthermore, the generation rate of medical waste was often reported as kg per (bed/day) by previous studies, and there was a lack of data for the generation rates of medical waste (GRMW) as kg per (patient/day).
2.2. Statistical Analysis
Analysis of variance (ANOVA) was conducted on quantitative data. This test evaluates the mean values of two or more groups of data to show whether the mean differences are significant or not. ANOVA is somehow the extension of the t-test. In the current study, ANOVA and boxplot were performed to show whether there was any significant difference in GRMW for different scenarios. The first scenario was the difference in GRMW before and during the COVID-19 pandemic. The second scenario investigated the difference in GRMW between the cities highly engaged in coronavirus compared to their country.
3. Results and Discussion
3.1. The Generation Rate of Medical Waste Before and During the COVID-19 Pandemic
The highest tonnage of medical waste was found in China before and during the COVID-19 pandemic (Tables 1 and 2). According to the current study, medical wastes were produced about 115, 444.8, 483.3, and 6067 tons/day in Malaysia, Iran, Bangladesh, and China, respectively. The amount of discharged facemasks in these countries was also estimated at 122, 309, 310, and 4214 tons/day (2). Only in Malaysia, the amount of facemask waste was higher than the daily tonnage of medical waste. This is probably because COVID-19 was not dominant in Malaysia when the daily amount of medical waste was reported. The highest GRMW was found at about 3.38 kg/(bed/day) in Tehran, Iran, before the pandemic, while the highest GRMW during the pandemic was observed in Dhaka at 4.8 kg/(bed/day). The GRMW from the largest to the lowest was observed to be 3.38, 2.98, 1.89, 1.55, 0.96, 0.71, and 0.56 kg/(bed/day) in Tehran, Iran, Bangladesh, Malaysia, Jordan, China, and Wuhan before the pandemic, respectively. However, during the pandemic, the descending GRMW was observed in Dhaka, Tehran, Bangladesh, Iran, Wuhan, Malaysia, and China with 4.8, 3.8, 3.4, 3.3, 2.94, 1.98, and 0.87 kg/(bed/day), respectively.
Table 1.
Tonnage and Generation Rates of Medical Waste per Day and Patients in Asia Before the COVID-19 Pandemic
|
Location
|
Period
|
Tons/day BC
|
kg/(bed/day) BC
|
kg/(day/
patient) BC
|
No. of Beds
|
No. of Patients
|
References
|
| KAUH, Jordan, Asia |
February–August 2004 |
0.087 |
0.29 |
0.36 |
300 |
242 |
(14)
|
| Jordan, Asia |
2003 |
9.4 |
0.96 |
- |
9743 |
- |
(15)
|
| Wuhan, China, Asia |
Before the pandemic |
50 |
0.56 |
- |
90 000 |
- |
(16)
|
| China, Asia |
Before the pandemic |
4903 |
0.71 |
- |
6 870 000 |
- |
(11,17)
|
| Malaysia, Asia |
Before the pandemic |
90 |
1.55 |
- |
58 000 |
- |
(18)
|
| Aradkuh, Tehran, Iran, Asia |
Before the pandemic |
87.4 |
3.38 |
- |
25 866 |
- |
(19,20,21)
|
| Iran, Asia |
2016 |
354.3 |
2.98 |
- |
118 894 |
- |
(19,20)
|
| DMCH, Bangladesh, Asia |
2006 |
3.27 |
1.93 |
0.63 |
1700 |
5200 |
(22)
|
| BMCH, Bangladesh, Asia |
2006 |
0.67 |
2.24 |
0.64 |
300 |
1050 |
(22)
|
| GH, Bangladesh, Asia |
2006 |
0.94 |
1.6 |
0.41 |
591 |
2289 |
(22)
|
Note. COVID-19: Coronavirus disease 2019; BC: Before COVID-19; KAUH: King Abdullah University Hospital; DMCH: Dhaka Medical College Hospital; BMCH: Bangladesh Medical College Hospital; GH: General hospitals.
Table 2.
Tonnage and Generation Rates of Medical Waste per Day and Patients in Asia during the COVID-19 Pandemic
|
Location
|
Period
|
Tons/day BC
|
Kg/(bed/day) DC
|
Kg/day/patient) DC
|
No. of Beds
|
COVID-19 Cases
|
References
|
| KAUH, Jordan, Asia |
March-20 |
0.395 |
3.95 |
14.16 |
100 |
28 |
(23,24)
|
| Wuhan, China, Asia |
Until March 2020 |
265 |
2.94 |
- |
90 000 |
50 333 |
(16)
|
| China, Asia |
Until March 21, 2020 |
6067 |
0.87 |
- |
6 960 000 |
82 100 |
(11,17,25)
|
| Malaysia, Asia |
Until March 2020 |
115 |
1.98 |
- |
58 000 |
3483 |
(18,25,26)
|
| Aradkuh, Tehran, Iran, Asia |
March 20 |
110 |
3.8 |
- |
29 254 |
~8369 |
(20,21,25)
|
| Iran, Asia |
April 22 |
444.8 |
3.3 |
- |
134 193 |
- |
(27)
|
| Dhaka, Bangladesh, Asia |
April 31, 2020 |
206 |
4.8 |
- |
42 571 |
~5701 |
(28,29,30)
|
| Bangladesh, Asia |
April 20 |
483.3 |
3.4 |
- |
141 903 |
7628 |
(25,28)
|
Note. COVID-19: Coronavirus disease 2019; BC: Before COVID-19; DC: During COVID-19; KAUH: King Abdullah University Hospital; DMCH: Dhaka Medical College Hospital; BMCH: Bangladesh Medical College Hospital; GH: General hospitals.
In the current study, GRMW was reported in three countries where one of their megacities presented its own GRMW during the pandemic. Accordingly, GRMW was lower in China, Iran, and Bangladesh compared to Wuhan, Tehran, and Dhaka, respectively, during the pandemic. The decreasing percentages were 70%, 13%, and 29% in Wuhan, Tehran, and Dhaka, respectively (Fig. 2). However, this trend was not followed in China before the pandemic, and GRMW in China (0.71 kg/(bed/day)) was larger than that in Wuhan (0.56 kg/(bed/day)). In all places, GRMW increased during the pandemic, and the most dramatic increase was observed in King Abdullah University Hospital in Jordan where the increased percentage was 1262%. On the other hand, one of the lowest increased percentages was observed in China by 23% after Tehran and Iran, suggesting that the larger place often results in a lower GRMW during a pandemic (Fig. 3). Fig. 3 presents strong descending trends of GRMW in all places based on the population, number of hospital beds, and accumulated COVID-19 cases during the pandemic. Although these trends were descending before the pandemic, no strong R2 (~0.03) was observed between GRMW and population or the number of hospital beds.
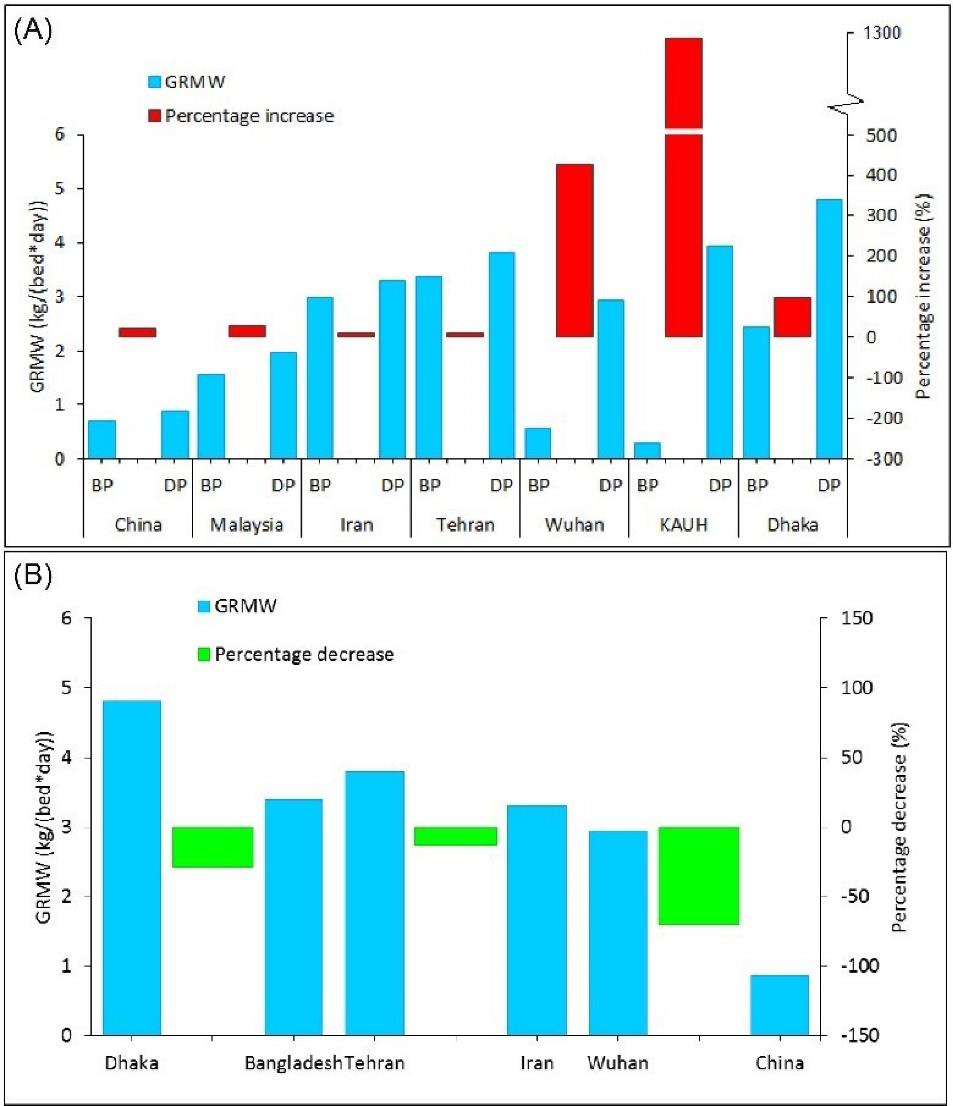
Fig. 2.
Percentage Increase of GRMW before the Pandemic in Asia (A) and GRMW in Countries and Their Mega Cities during the Pandemic (V). Note. GRMW: Generation rate of medical waste; BP: Before the pandemic: DP: During the pandemic
.
Percentage Increase of GRMW before the Pandemic in Asia (A) and GRMW in Countries and Their Mega Cities during the Pandemic (V). Note. GRMW: Generation rate of medical waste; BP: Before the pandemic: DP: During the pandemic
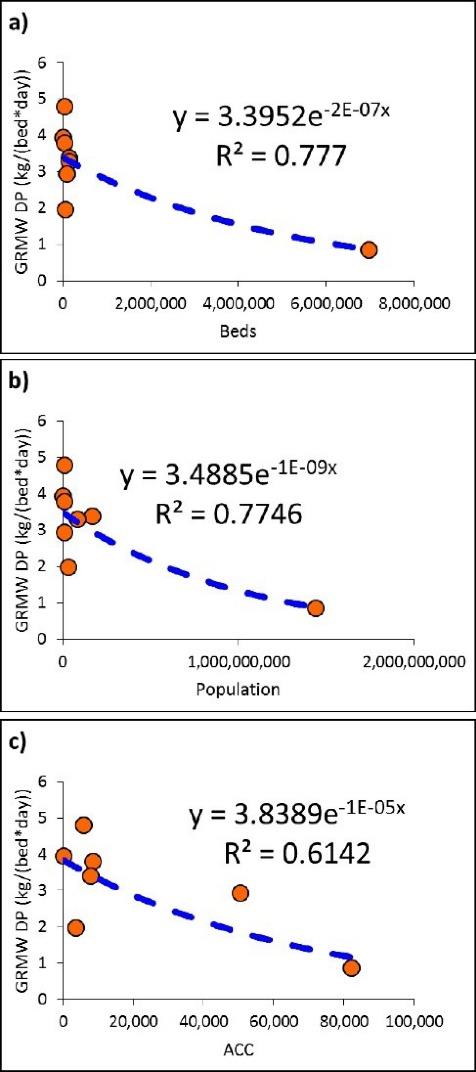
Fig. 3.
The Trend of GRMW based on the Hospital Beds (a), Population (b), and ACC (c) during the COVID-19 Pandemic. Note. GRMW: Generation rate of medical waste; ACC: Accumulated confirmed cases; COVID-19: Coronavirus disease 2019
.
The Trend of GRMW based on the Hospital Beds (a), Population (b), and ACC (c) during the COVID-19 Pandemic. Note. GRMW: Generation rate of medical waste; ACC: Accumulated confirmed cases; COVID-19: Coronavirus disease 2019
The statistical analysis of medical waste before and during the pandemic is presented in Table 3 and Fig. 4. Based on the analysis of variance, the F-value was greater than 4 only between GRMW before and during the pandemic; however, the corresponding P value was insignificant. Likewise, the total generation of medical waste per day did not display any significant difference before and during the pandemic. The difference in GRMW between megacities and their countries was similarly insignificant during the pandemic in Asia. These results are also graphically presented in Fig. 4 by box plots.
Table 3.
ANOVA for the GRMW before and during the Pandemic and for the GRMW Between Countries and Their Mega Cities During the Pandemic
|
Different Scenarios of Medical Waste Generation
|
F
|
P
Value
|
| GRMW before and during the pandemic |
4.12 |
0.065 |
| TGMW before and during the pandemic |
0.04 |
0.846 |
| Engaged mega cities versus their countries |
1.8 |
0.251 |
Note. ANOVA: One-way analysis of variance; GRMW: Generation rate of medical waste; TGMW: Total generation of medical waste.
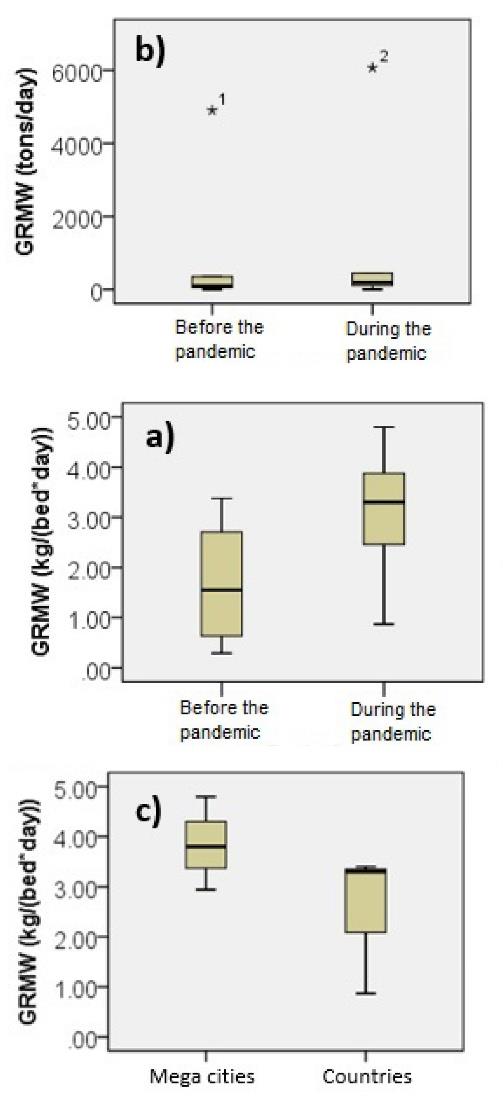
Fig. 4.
Box Plots of GRMW Before and During the Pandemic (a, b) and of the GRMW Between Countries and Their Mega Cities during the Pandemic (c). Note. GRMW: Generation rate of medical waste
.
Box Plots of GRMW Before and During the Pandemic (a, b) and of the GRMW Between Countries and Their Mega Cities during the Pandemic (c). Note. GRMW: Generation rate of medical waste
3.2. Disinfecting Methods of Medical Wastes During the Coronavirus Disease 2019 Pandemic
3.2.1. Autoclaving
Autoclave includes the disinfection of wastes by exposing them to direct steam at temperature, pressure, and contact time around 121-134°C, 15 Psi, and 30-60 minutes, respectively. Each cycle of autoclaving is completed with 200 to 10 000 L of waste. Sharp tools, reusable instruments, bedding wastes, and personal protective equipment are often persuaded to use autoclaves. This method is not recommended for the disinfection of chemical, radioactive, volatile, and semi-volatile wastes. Autoclave does not reduce the volume of the wastes, so complementary treatment of the autoclaved wastes is required. It is difficult to kill all microorganisms for large quantities of the wastes as well as large wastes (2,31,32).
3.2.2. Microwaves
Wastes are irradiated by electromagnetic waves from microwaves with length waves between 200-300 nm. Each cycle with 30-500 liters of waste is completed in 30-60 minutes. The wastes should have enough water to complete the thermal process. This method is also applied to the same wastes that are disinfected by autoclave. The microwave process heats the waste from inside to outside, and it is not economical to treat large quantities of waste with microwaves (2,33).
3.2.3. Chemical Disinfecting
Chemical disinfection, sodium hypochlorite, calcium hypochlorite, dioxide chloride, proxy acid, ozone, dry lime, and iron catalyzers are frequently used with crushed wastes. The wastes are crushed due to the increase in contact surface and mixed with chemical disinfectants. Therefore, microorganisms are killed after an effective contact time. This method is rapid and stable for disinfecting a wide range of wastes although residual of the process, costs, and well-trained experts are considered disadvantages of this technology (34).
3.2.4. Landfilling
Landfilling is the easiest method for disposing the waste with low costs. The potential of public health and environmental issues will rise if the technology utilizes an open dump approach (35,36). Stabilized and degraded solid wastes, leachate, and gas (i.e., CO2, H2S, CH4, and the like) are the final productions of landfilling even though air, soil, and water are contaminated. Therefore, landfilling of medical wastes is not recommended and correct. The disposal of medical wastes in landfills should be prohibited in many countries unless the medical waste is disinfected from all hazardous microorganisms so that exposure to them does not cause any health and environmental issues (1,37).
3.2.5. Incineration
Incineration technology applies dry oxidation at temperatures higher than 850°C for the treatment of the wastes. The capacity and cycling time of the incinerations range between 15-2000 kg/h and 6-8 hours. Due to the high temperature of the process, infectious wastes are effectively treated. The unreusable and unrecyclable wastes are the input of the incinerations before being disposed in landfills. This method considerably decreases the volume of the wastes and turns them into ash and gas. In addition to the advantages of incinerators, they also led to many human and environmental concerns since they release heavy metals, dioxin, furan, hydrogen chloride, and the like into the atmosphere (38,39). In general, the most used technologies were autoclaves and microwaves for disinfecting the medical wastes in Asia. Over 80% of infectious wastes were disinfected by autoclave and microwave in India, while at the worst case, the percentage use of autoclave and microwave was about 60% in Bangladesh (Table 4). Moreover, the incinerators were used less frequently in Asia, and their frequency percentage was around 5%.
Table 4.
Frequency Percentage of the Used Disinfecting Methods in Different Countries
|
Countries
|
Autoclave
|
Microwave
|
Chemical Disinfecting
|
Landfilling
|
Incinerators
|
| India |
43 |
39 |
10 |
6 |
2 |
| Malaysia |
41 |
38 |
8 |
7 |
6 |
| China |
38 |
37 |
12 |
10 |
3 |
| Australia |
43 |
32 |
11 |
7 |
7 |
| Bangladesh |
31 |
27 |
16 |
18 |
8 |
4. Conclusion
In this study, the relationship between COVID-19 incidences and medical wastes as well as recommended disinfecting methods were reviewed and analyzed. It was found that GRMW increased in all hospitals, cities, and countries during the pandemic period in Asia. According to the results of the ANOVA test, this increase was almost significant because the F-value was greater than 4, while the P value was not lower than 0.05. When considering the whole country, its GRMW is lower compared to the most engaged city. Furthermore, an increase in hospital beds, population, and accumulated confirmed cases of COVID-19 led to a decrease in GRMW. Autoclaves and microwaves were considered the most popular techniques for disinfecting medical wastes, while the least popular methods were chemical disinfecting, landfilling, and incinerators.
The investigation of the same study is recommended for other continents as future works. Comparing the results of such studies in different continents may reveal interesting features. Since medical wastes are produced differently from patient to patient, the evaluation of GRMW as unit of kg/patient/day is also suggested.
Acknowledgments
The authors thank Ahvaz Jundishapur University of Medical Sciences and Mizan Online News Agency for educational support and information about medical waste.
Authors’ Contribution
Conceptualization: Heydar Maleki, Nematollah Jafarzadeh.
Data curation: Heydar Maleki.
Investigation: Heydar Maleki, Nematollah Jafarzadeh.
Methodology: Heydar Maleki.
Project administration: Nematollah Jafarzadeh.
Resources: Heydar Maleki.
Software: Heydar Maleki.
Writing–original draft: Heydar Maleki.
Writing–review & editing: Heydar Maleki, Nematollah Jafarzadeh.
Competing Interests
The authors declare that they do not have any conflict of interests.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethical Approval
Not applicable.
Funding
This study is part of personal research, and no funding was provided.
References
- Hossain MS, Santhanam A, Nik Norulaini NA, Omar AK. Clinical solid waste management practices and its impact on human health and environment--a review. Waste Manag 2011; 31(4):754-66. doi: 10.1016/j.wasman.2010.11.008 [Crossref] [ Google Scholar]
- Hantoko D, Li X, Pariatamby A, Yoshikawa K, Horttanainen M, Yan M. Challenges and practices on waste management and disposal during COVID-19 pandemic. J Environ Manage 2021; 286:112140. doi: 10.1016/j.jenvman.2021.112140 [Crossref] [ Google Scholar]
- Bdour A, Altrabsheh B, Hadadin N, Al-Shareif M. Assessment of medical wastes management practice: a case study of the northern part of Jordan. Waste Manag 2007; 27(6):746-59. doi: 10.1016/j.wasman.2006.03.004 [Crossref] [ Google Scholar]
- Mahmudiono T, Ramaiah P, Maleki H, Doewes RI, Shalaby MN, Alsaikhan F. Evaluation of the impact of different disinfectants on new coronavirus and human health. Rev Environ Health 2023; 38(3):451-60. doi: 10.1515/reveh-2022-0051 [Crossref] [ Google Scholar]
- Sarkodie SA, Owusu PA. Impact of COVID-19 pandemic on waste management. Environ Dev Sustain 2021; 23(5):7951-60. doi: 10.1007/s10668-020-00956-y [Crossref] [ Google Scholar]
- Neisi A, Goudarzi G, Babaei A, Hamid V, Mousavi SK, Kanani P. Meta-analysis of COVID-19 spread in meat processing plants and recommended practical actions. Avicenna J Environ Health Eng 2022; 9(2):109-16. doi: 10.34172/ajehe.2022.5270 [Crossref] [ Google Scholar]
- Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect 2020; 104(3):246-51. doi: 10.1016/j.jhin.2020.01.022 [Crossref] [ Google Scholar]
- van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 2020; 382(16):1564-7. doi: 10.1056/NEJMc2004973 [Crossref] [ Google Scholar]
- World Health Organization. Waste Management during the COVID-19 Pandemic. IGES Center Collaborating with UNEP on Environmental Technologies (CCET); 2020.
- Nzediegwu C, Chang SX. Improper solid waste management increases potential for COVID-19 spread in developing countries. Resour Conserv Recycl 2020; 161:104947. doi: 10.1016/j.resconrec.2020.104947 [Crossref] [ Google Scholar]
- Singh N, Tang Y, Zhang Z, Zheng C. COVID-19 waste management: effective and successful measures in Wuhan, China. Resour Conserv Recycl 2020; 163:105071. doi: 10.1016/j.resconrec.2020.105071 [Crossref] [ Google Scholar]
- World Bank. Solid Waste Management. 2019. Available from: https://www.worldbank.org/en/topic/urbandevelopment/brief/solid-waste-management. Accessed July 14, 2020.
- Ferronato N, Torretta V. Waste mismanagement in developing countries: a review of global issues. Int J Environ Res Public Health 2019; 16(6):1060. doi: 10.3390/ijerph16061060 [Crossref] [ Google Scholar]
- Abu Qdais H, Rabi A, Abdulla F. Characteristics of the medical waste generated at the Jordanian hospitals. Clean Technol Environ Policy 2007; 9(2):147-52. doi: 10.1007/s10098-006-0077-0 [Crossref] [ Google Scholar]
- Alnatsheh B. Medical waste management. In: Proceedings of the Workshop on Proper Management Practices of the Medical Waste. Irbid, Jordan: Rahma Hospital; 2004.
- Chen Y, Guo C. Handbook of Emergency Disposal and Management of Medical Waste in China. Royal Collins Publishing Company; 2020.
- Number of hospital beds in China 2011-2021. https://www.statista.com/statistics/279370/number-of-hospital-beds-in-china/.
- Astro Awani. COVID-19: Clinical Waste Management Still Under Control-Dr Noor Hisham. Available from: http://english.astroawani.com/. Accessed May 25, 2020.
- Eslami A, Nowrouz P, Sheikholeslami S. Status and challenges of medical waste management in hospitals of Iran. Civ Eng J 2017; 3(9):741-8. doi: 10.21859/cej-030910 [Crossref] [ Google Scholar]
- Mosadeghrad AM, Janbabaei G, Kalantari B, Darrudi A, Dehnavi H. Equity in distribution of hospital beds in Iran. Sci J Kurdistan Univ Med Sci 2020; 24(6):12-36. doi: 10.29252/sjku.24.6.12.[Persian] [Crossref] [ Google Scholar]
- Mizan online news Agency website. https://www.mizan.news.
- Hassan MM, Ahmed SA, Rahman KA, Biswas TK. Pattern of medical waste management: existing scenario in Dhaka city, Bangladesh. BMC Public Health 2008; 8:36. doi: 10.1186/1471-2458-8-36 [Crossref] [ Google Scholar]
- Abu-Qdais HA, Al-Ghazo MA, Al-Ghazo EM. Statistical analysis and characteristics of hospital medical waste under novel coronavirus outbreak. Glob J Environ Sci Manag 2020; 6(SI):21-30. doi: 10.22034/gjesm.2019.06.si.03 [Crossref] [ Google Scholar]
- King Abdullah University Hospital (KAUH). 2002. https://www.linkedin.com/company/kauh/about/.
- Malaysia – COVID-19. https://covid19.who.int/region/wpro/country/my.
- Agamuthu P, Barasarathi J. Clinical waste management under COVID-19 scenario in Malaysia. Waste Manag Res 2021; 39(1_suppl):18-26. doi: 10.1177/0734242x20959701 [Crossref] [ Google Scholar]
- Daily production of 444 tons of medical waste in the country. https://saatesalamat.ir/1401021902-2/.
- Rahman MM, Bodrud-Doza M, Griffiths MD, Mamun MA. Biomedical waste amid COVID-19: perspectives from Bangladesh. Lancet Glob Health 2020; 8(10):e1262. doi: 10.1016/s2214-109x(20)30349-1 [Crossref] [ Google Scholar]
- Khan MH, Howlader T, Islam MM. Battling the COVID-19 pandemic: is Bangladesh prepared? medRxiv [Preprint]. May 12, 2020. Available from: https://www.medrxiv.org/content/10.1101/2020.04.29.20084236v2.
- Akter N, Tränkler J. An analysis of possible scenarios of medical waste management in Bangladesh. Manag Environ Qual 2003; 14(2):242-55. doi: 10.1108/14777830310470459 [Crossref] [ Google Scholar]
- Lee BK, Ellenbecker MJ, Moure-Ersaso R. Alternatives for treatment and disposal cost reduction of regulated medical wastes. Waste Manag 2004; 24(2):143-51. doi: 10.1016/j.wasman.2003.10.008 [Crossref] [ Google Scholar]
- Jang YC, Lee C, Yoon OS, Kim H. Medical waste management in Korea. J Environ Manage 2006; 80(2):107-15. doi: 10.1016/j.jenvman.2005.08.018 [Crossref] [ Google Scholar]
- Cha CY, Carlisle CT. Microwave process for volatile organic compound abatement. J Air Waste Manag Assoc 2001; 51(12):1628-41. doi: 10.1080/10473289.2001.10464389 [Crossref] [ Google Scholar]
- Wang J, Shen J, Ye D, Yan X, Zhang Y, Yang W. Disinfection technology of hospital wastes and wastewater: suggestions for disinfection strategy during coronavirus disease 2019 (COVID-19) pandemic in China. Environ Pollut 2020; 262:114665. doi: 10.1016/j.envpol.2020.114665 [Crossref] [ Google Scholar]
- Butt TE, Lockley E, Oduyemi KO. Risk assessment of landfill disposal sites--state of the art. Waste Manag 2008; 28(6):952-64. doi: 10.1016/j.wasman.2007.05.012 [Crossref] [ Google Scholar]
- Narayana T. Municipal solid waste management in India: from waste disposal to recovery of resources?. Waste Manag 2009; 29(3):1163-6. doi: 10.1016/j.wasman.2008.06.038 [Crossref] [ Google Scholar]
- Nema SK, Ganeshprasad KS. Plasma pyrolysis of medical waste. Curr Sci 2002; 83(3):271-8. [ Google Scholar]
- WHO WHO. Safe healthcare waste management-policy paper by the World Health Organization. Waste Manag 2005; 25:568-9. [ Google Scholar]
- Ananth AP, Prashanthini V, Visvanathan C. Healthcare waste management in Asia. Waste Manag 2010; 30(1):154-61. doi: 10.1016/j.wasman.2009.07.018 [Crossref] [ Google Scholar]