Avicenna J Environ Health Eng. 9(2):109-116.
doi: 10.34172/ajehe.2022.5270
Systematic Review
Meta-Analysis of COVID-19 Spread in Meat Processing Plants and Recommended Practical Actions
Abdolkazem Neisi 1  , Gholamreza Goudarzi 1, Aliakbar Babaei 1, Vafa Hamid 2, Seyede Kosar Mousavi 2, Parnia Kanani 2, Niloufar Lajmorak 2, Heydar Maleki 2, *
, Gholamreza Goudarzi 1, Aliakbar Babaei 1, Vafa Hamid 2, Seyede Kosar Mousavi 2, Parnia Kanani 2, Niloufar Lajmorak 2, Heydar Maleki 2, * 
Author information:
1Department of Environmental Health Engineering, School of Health, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
2Department of Environmental Health Engineering, School of Health, Student Research Committee, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
Abstract
Recently, the spread of the coronavirus disease 2019 (COVID-19) has increased among workers of meat processing plants (MPPs) around the world. This study reviewed the possible routes of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission and useful actions against it in slaughterhouses. The results revealed that the main factors for the spread of the virus included low indoor temperature, crowded area, wrong standing along production lines, contamination of high-touch surfaces, difficult education of workers with diverse native languages, low financial income, large MPPs with over 10 million Ib of packed meat per month, higher speed of production lines with 175 birds/minute, temporary contract of the workers, and weak approach of some meat processing companies against COVID-19 infection such as National Beef. COVID-19 transmission rate was 24 times higher among the workers of MPPs than among the population of the US. The practical actions against the spread of the virus were mainly marker using for remembering the previous location, mandatory mask use, especially FFP2/3 masks, and decentralization of large MPPs. By using the results of this study, slaughterhouse managers would be able to significantly control the spread of SARS-CoV-2 and future bio-threats to workers of MPPs and even to society.
Keywords: COVID-19, Meat processing plants, Transmission routes, Practical actions, High-touch surface,
Copyright and License Information
© 2022 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Please cite this article as follows: Neisi A, Goudarzi G, Babaei A, Hamid V, Mousavi SK, Kanani P, et al. Meta-analysis of COVID-19 spread in meat processing plants and recommended practical actions. Avicenna J Environ Health Eng. 2022; 9(2):109-116. doi:10.34172/ajehe.2022.5270
1. Introduction
In spite of the spread of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection through respiratory system, it can enter the body through other routes. Upon the entry, angiotensin-converting enzyme 2 (ACE2), receptor of novel coronavirus, indicated significant correlations with alveolar epithelial II, epithelial cells, and epithelial enterocytes (1-3). Many studies demonstrated the existence of the virus through whole gastrointestinal tract during the SARS-CoV-2 pandemic (4). It was found that the spread of the coronavirus disease 2019 (COVID-19) is possible through non-droplet transmission. Further, the existence of the coronavirus in feces exhibited significant correlation with gastrointestinal discomfort (5,6).
Airborne transmission is possible during flushing the toilet (7,8). Generating fecal aerosols containing Torque teno and adenoviruses were previously recorded in toilets (9). Recent studies also suggested that COVID-19 could spread through fecal aerosol (10,11). Moreover, the existence of the new coronavirus was potentially analyzed through paper-based devices in municipal wastewater for prediction of upcoming outbreak that could be cheaper than polymerase chain reaction (PCR) test (12).
Oral transmission of coronavirus was previously observed through the Middle East respiratory syndrome coronavirus. Direct contact with respiratory droplets or salvia of camels, drinking unpasteurized milk, or eating undercooked meat resulted in the Middle East respiratory syndrome coronavirus infection (13,14). The novel coronavirus is suspected for possible distribution in meat processing facilities (15) and then correlated directly with the number of infectious patients (16). At the beginning of COVID-19 pandemic, the United States experienced the largest epicenters of COVID-19 outbreaks in meat processing facilities (17). Dozens of employees were diagnosed with COVID-19 in South Dakota, USA, Gütersloh in Germany, and Alberta in Canada (18). The distinctive reasons for being vulnerable against COVID-19 infection in meat processing plants (MPPs) are close contacts ( < 2 meters), contact time, type of transmission, low temperature, and different cultural backgrounds. Regarding close contacts, it was observed that employees alongside production lines work close to each other with a distance of less than two meters. In addition, locker rooms and break times increased the possibility of close contacts (19). In terms of contact time, workers in meat processing facilities were found to work 10 to 12 hours per shift which increased the risk of transmission through continuous contacts (20,21). With respect to the type of transmission, workers may be infected by breathing droplets due to loud talking, sneezing, and coughing or by touching contaminated objects or surfaces (15,18). Another reason is attributed to low temperature. Since many parts of slaughterhouses have low temperature due to food maintenance, coronavirus can survive for a longer period of time compared with room temperature (18,22). Moreover, since considerable portion of employees in MPPs are from different cultural backgrounds, it would be difficult to explain the educational and protective regulations to them (23,24).
Since a dozen of studies evaluated the effect of COVID-19 in MPPs through limited aspects, it seems necessary to provide a study containing relevant aspects all together. In addition, the above-mentioned studies were all conducted in Europe and North America; therefore, the present study could provide a good guideline for managing MPPs in other continents. In this study, all associated papers and documents that represented a clue about the two mentioned issues were reviewed chronologically to demonstrate the current situation of MPPs.
2. Materials and Methods
2.1. Study Design
All published papers and reports that evaluated the relationship between the COVID-19 incidence and MPPs were gathered and reviewed to present a clear status of SARS-CoV-2 in slaughterhouses. The documents and data were gathered from Web of Science, Scopus, PubMed, Google Scholar, newspaper websites, as well as Worldometers and Macrotrends websites. The study was conducted based on the all relevant documents published until 1 July 2021. In the first step, the following items were used to find documents associated with food, COVID-19 exposure, COVID-19 transmission, COVID-19 cases and deaths, meat, large markets, fish, salmon, MPPs, the US, Germany, Netherlands, ventilation, air temperature, relative humidity, contaminated surface, and airborne transmission (Fig. 1). Based on the search items, the identification phase was completed by 102 documents. After title and abstract checking, 44 documents were found with irrelevant scope, which were removed through screening step. Moreover, 10 out of the 61 remaining documents were also removed in eligibility phase because they were written in other languages, or after reading the whole document, it was revealed that they generalized the stability of SARS-CoV-2 in different places which were not related to MPPs. In other words, documents that specifically evaluated and illustrated the situation of MPPs during COVID-19 outbreak were eligible and selected. Finally, 30 documents were included in results and discussion sections, and the current study systematically evaluated their data and findings. The result of the study was reviewed in four subsections: 1) Environmental variables related to the stability of SARS-CoV-2 in slaughterhouses; 2) Food safety and COVID-19 transmission in slaughterhouses; 3) Different secretions and COVID-19 transmission in slaughterhouses; and 4) Practical actions against COVID-19 in slaughterhouses. Section 2 chronologically reviewed the documents to demonstrate the infection of SARS-CoV-2 in MPPs all over the world. This study only used English documents. However, there were some Chinese reports that seemed useful to utilize in the study, but language limitation of the authors for Chinese translation led to their elimination. Another limitation of the current study was using data sources with different structures since newspapers often qualitatively reported the information, while scientific papers reported information more quantitatively. Therefore, it was difficult to evaluate them by the same pattern.
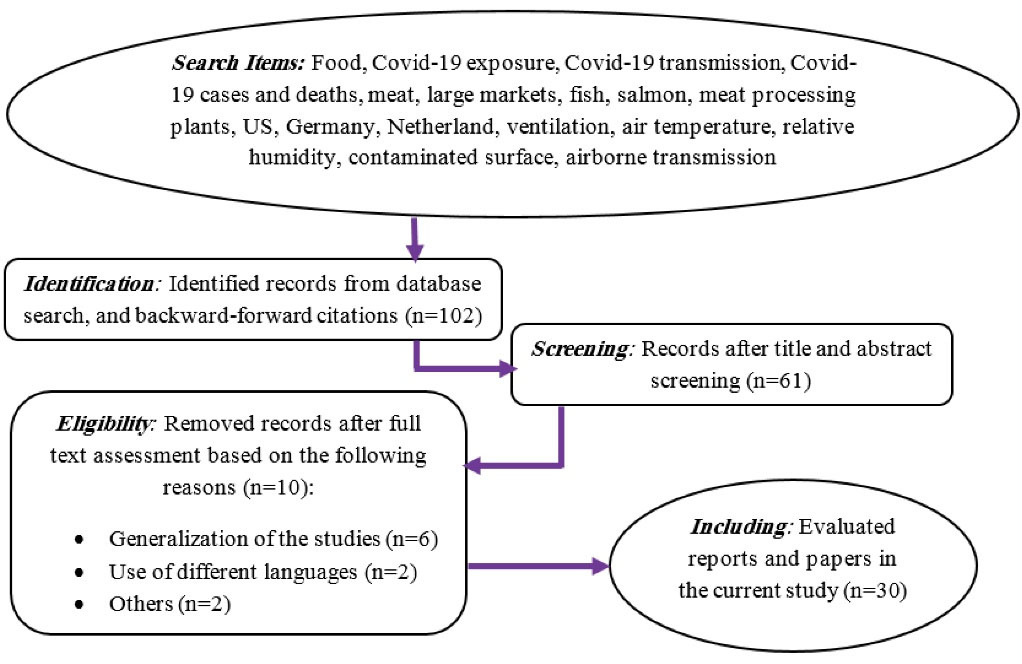
Fig. 1.
Preferred Reporting Items for Meta-analysis Flow Diagram of the Current Study
.
Preferred Reporting Items for Meta-analysis Flow Diagram of the Current Study
3. Results and Discussion
3.1. Environmental Variables Related to Stability of SARS-CoV-2 in Slaughterhouses
Survival from COVID-19 mainly lasts less than a week, and the survival time depends highly on the types of objects. The virus even cannot multiply on the surface of food packages. Therefore, the infectious droplets decrease in number over time on surfaces. It is also limited mainly by basic actions like surface disinfectant (25,26). According to WHO findings, SARS-CoV-2 is more likely to survive in laboratory conditions compared to other types of coronaviruses. Additionally, the virus survived more than two days in urine and feces at room temperature. The stability of the virus will increase until four days if the feces have higher pH. It should be noted that cultivation of the virus at 4°C and 80°C did not show any quantitative significant difference after 21 days (27). However, Duan et al found that SARS viruses survived longer days at 4°C than 25°C.
SARS-CoV-2 was stable about 4 days on plastic surface at room temperature with relative humidity around 46%, and its infectious feature could be totally disabled after seven days (28). van Doremalen et al demonstrated that COVID-19 stability on plastic surface was three days at room temperature in which it could not be infectious after four days. They also revealed that the stability time of SARS-CoV-2 and SARS-CoV-1 was the same on plastic objects. Compared to SARS-CoV-1, the novel coronavirus was active for shorter time on copper objects. Generally, survival of coronaviruses on zinc and stainless steel surfaces was longer than survival on nickel, brass, and copper objects (29). A study on glass showed that SARS-CoV-2 remained stable after two days at 25°C and 65% relative humidity, and it completely degraded after four days (28). Since clothes are made of porous materials, they are not a possible route for COVID-19 transmission (30).
It was found that the immune system cannot remove SARS-CoV-2, and the spread of the virus was potentially high through asymptomatic infection (29,31,32). Half-lives of the novel coronavirus and SARS-CoV-1 were detected to be the same on copper objects and in aerosol. Although, half-life of SARS-CoV-2 on cardboard was recorded to be longer than that of SARS-CoV-1, half-lives of the new virus and SARS-CoV-1 were estimated to be around 5.6 hours and 4.2 hours on stainless steel surfaces and 6.8 hours and 7.6 hours on plastic objects, respectively (29). Therefore, being infected with COVID-19 is possible through both droplets and contaminated surfaces.
3.2. Food Safety and COVID-19 Transmission in Slaughterhouses
It was previously found that not only food and meat were not associated with the transmission of SARS-CoV-2 (33) but also food and meat packaging prevented the spread of other diseases (34). Recently, COVID-19 spread has been correlated with the biggest agricultural and seafood market, Xinfadi. The collected samples from salmon in Xinfadi were positive for the presence of SARS-CoV-2. The main routes of transmission were suggested to be through breathing droplets and touching surfaces. To prevent the spread of the virus, it was suggested to eat completely cooked food, and indirectly have contact with raw fish and meat (35). The annual rate of imported salmon to China is about 80 000 tons per year, which can increase annually. In another report, it was detected that frozen salmon had active SARS-CoV-2 at Xinfadi market. It was noted that the live salmon could not be a source of COVID-19, but some active cells of chilled salmon could be the routes of transmission. This was mainly because of the contaminated environment for salmon processing, packaging, and transportation (36).
Slaughterhouses (i.e., houses for pigs, poultry, and cattle) were detected as one of the corresponding factors for half of the SARS-CoV-2 infections in the US (37). The majority of infected employees were mainly from ethnic minority workers and migrants (38). About 40% (66 employees) of infected people consisted of Romanian and Polish workers in pig processing facilities in Netherlands (39). The cutting and deboning areas contained 21% and 50% of the positive SARS-CoV-2 tests among the employees, respectively. Moreover, 3 out of 22 surface samples in productive sections and 3 out of 17 samples in non-productive areas demonstrated active presence of SARS-CoV-2 on high-touch tools in slaughterhouses (39). It was also revealed that mean indoor air temperature was around 6°C in MPPs. The number of infected workers was close to each other in Pokora et al (40) and Herstein et al’s (41) studies, while the numbers of investigated MPPs were 22 and 13 in these studies. Effect of ventilation (i.e., 364-1885 m3/(employee* hour)) is probably the reason that the number of infected workers in 22 MPPs in Gemany was the same as the number of workers in 13 MPPs in the US. In addition, 11% of collected samples in Razi hospital in Ahvaz were positive for the presence of SARS-CoV-2 where ventilation systems did not work (42). The majority of studies illustrated that MPP staff were mostly infected symptomatically (Table 1). According to Waltenburg et al’ s study, the ratio of confirmed COVID-19 cases per number of MPP workers in the US was 0.144 until May 31, 2020, while the general ratio of confirmed COVID-19 cases (1 907 370) in the US per its 2020-population (331 002 651) was 0.006 until May 31, 2020 (43,44). Therefore, as presented in Fig. 2, a significance difference was found between the ratios in MPPs and the whole country.
Table 1.
Main Features of Poultry and MPPs Across the World During the Study Period
|
Type of MPPs
|
Country, City
|
Study Period
|
T (°C)
|
RH (%)
|
Ventilation
|
No. of Infected Workers or People
|
Symptoms Type
|
Action
|
Reference
|
| Beef, bison, lamb, pork, poultry, and veal processing plants |
23 states in the US |
April-May 2020 |
- |
- |
- |
16233 (14.4% of all workers) |
Symptomatic (90%) and Asymptomatic (10%) |
Proper and regular use of personal protective equipment, workers’ temperature screening and physical barriers; Hispanic workers were the most at risk workers. |
(15) |
| Meat processing facilities and large meatpacking companies |
The US |
July-2020 |
0-12 |
90-95 |
- |
270000 infected cases and 4700 deaths |
- |
Shifting to more decentralization of large MPPs |
(17) |
| MPPs |
The US, Canada, Germany, France, Spain, and the UK |
March-June 2020 |
Low |
- |
- |
150+ workers in Anglesey, Wales |
- |
Cleaning floors with sluice water and rubber squeegees rather than brushes and hoses; Use of FFP2/3 masks; regular screening of the workers |
(18) |
| Major supermarkets |
Beijing, China |
before June 2020 |
- |
- |
- |
No one |
- |
Avoiding from directly touching fish and meat |
(35) |
| Major supermarkets and sushi restaurant |
Beijing, China |
before June 2020 |
- |
- |
- |
Low number of wholesalers |
- |
Preventing from selling salmon |
(36) |
| Large pig processing plant |
Netherlands |
June-2020 |
5-9 |
- |
- |
27 out of 76 |
Dominantly asymptomatic |
8-meter distance in production rooms and good ventilation systems; |
(39) |
| 22 meat and poultry plants |
Germany |
June-September 2020 |
2-12+ |
- |
364-1885 m3/ (employee* hour) |
6522 |
- |
Increasing the amount of outdoor air flow per employee in different working area in MPPs; More important role of outdoor air flow per employee than air temperature was observed. |
(40) |
| 13 MPPs |
Nebraska, The US |
April-July 2020 |
Low |
- |
- |
5002 |
Symptomatic (85%) |
Use of masks by all employees and physical partitioning significantly reduced COVID-19 cases in 8 out 13 MPPs. |
(41) |
| Meat and poultry facilities |
The US, Canada, Ireland, Germany, Australia, France, Brazil, and Spain |
Before May 2020 |
4-6 |
> 50 |
- |
> 15689 |
- |
Proper and regular use of personal protective equipment |
(45) |
| A questionnaire from MPP workers |
The US |
May-2020 |
- |
- |
- |
244 |
Symptomatic (52%) |
Proper and regular use of personal protective equipment and physical barriers; The MPP managers only care about meat production not health of workers. |
(46) |
Note. MPPs: Meat processing plants; T: Air temperature; RH: Relative humidity; COVID-19: Coronavirus disease 2019.
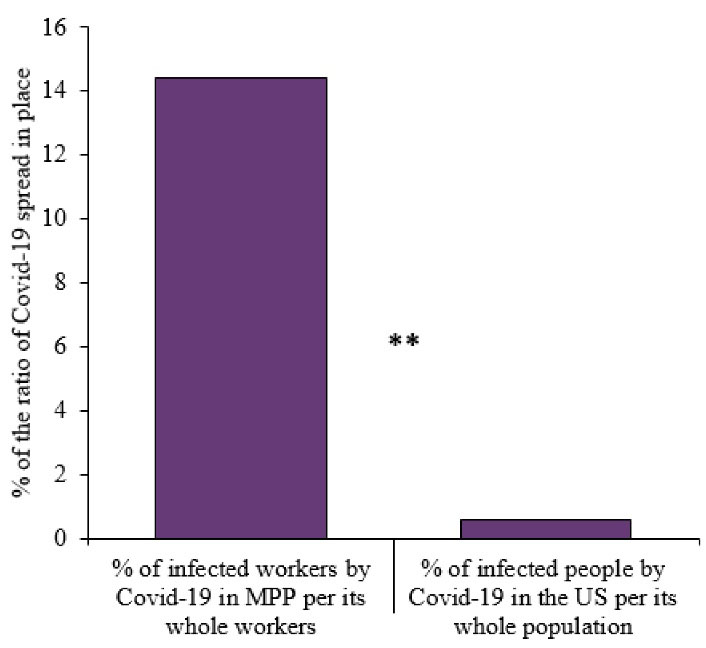
Fig. 2.
Percentage of the Ratios of Confirmed COVID-19 Cases Among the MPP Workers and the Whole US Population Until May 31, 2020. Note. COVID-19: Coronavirus disease 2019; MPP: Meat processing plant
.
Percentage of the Ratios of Confirmed COVID-19 Cases Among the MPP Workers and the Whole US Population Until May 31, 2020. Note. COVID-19: Coronavirus disease 2019; MPP: Meat processing plant
As observed, there was a significant and direct correlation between infected cases in slaughterhouses and the spread of SARS-CoV-2 in the US. Increased COVID-19 cases and associated deaths were demonstrated about 7% (270 000 cases) and 3.5% (4750 deaths) in the US due to polluted MPPs (17). It was also found that large meat processing and packaging plants had higher association with the spread of SARS-CoV-2. Further, counties that had plants with processing rate over 10 million Ib of meat per month present 35% higher cases of COVID-19 compared to other counties, while no significant correlation was found between COVID-19 cases and plants with processing rate of one million Ib of meat per month. Moreover, closure of MPPs led to reduction of COVID-19 cases. Increasing the speed of production lines also caused higher infected cases in counties. Poultry plants in the US have been allowed to increase the speed of production lines from 140 birds per minute to 175 since 2018. Accordingly, the spread of SARS-CoV-2 virus was two times higher in cities that increased the speed of production lines compared to cities with previous speed of production lines. In addition, the spread of SARS-CoV-2 was detected to be different even among meat processing companies including National Beef, JBS, Tyson, Cargill, and Smithfield. Further, the COVID-19 incidence rate in National Beef was five times higher than that in other meat processing companies (17).
Incidence of COVID-19 cases was observed to be about 12% in seven MPPs in Germany. The highest percent was 16% in cutting and deboning sections. Improving ventilation rate, physical distancing, and rooms with high temperature resulted in lower infections of the virus. Although medical masks were the most frequent type of face covering in all slaughterhouses, plants in which the majority used FFP2 masks demonstrated no infected workers. The type of employees’ contract also showed significant difference in terms of COVID-19 incidences. Accordingly, the infectious rate of SARS-CoV-2 was 71% higher among workers with temporary contracts than that of workers with permanent contract (40).
3.3. Different Secretions and COVID-19 Transmission in Slaughterhouses
The novel coronavirus is mainly transmitted through high-touch contaminated surfaces (47). The contaminating approaches are fecal-oral transmission and breathing droplets. SARS-CoV-2 could spread during eating food or drinking beverage since they can be contaminated by infectious feces (6). It can also be transmitted through respiratory droplets which are the result of loud talking, sneezing, and coughing in MPPs (45). Workers usually talk loudly in MPPs because the constant sound of processing machines prevent them from hearing normal conversation, and the minimum sound level in MPPs belongs to packing equipment rooms with 85 dB (18,40); furthermore, large processing rooms persuade workers to talk loudly (17). Durand-Moreau et al investigated the use of laser light scattering to depict each droplet as one flash. They found that there is a direct relationship between the number of flashes (i.e., droplets) and the loudness of staff conversations (45). Other studies also revealed that breathing droplets could lead to the infection with COVID-19 among people who are close to each other (i.e., distance of no less than 1.5 meters) (26). Infected tools such as thermometer also yielded the same result (48,49).
Moreover, common washing and brushing of the floors and surfaces by high-pressure water increased the generation rate of droplet and aerosol in MPPs. Aerosolization of the novel coronavirus would be an unwelcomed result of washing contaminated surfaces using such procedures. In addition, MPPs have chilly environment that causes longer period of exposure to airborne infection of SARS-CoV-2 (18). A study in the Netherlands reported less significant levels of SARS-CoV-2 through air samples of cooled environments in slaughterhouses. Moreover, active viruses were detected through stationary atmospheric samples from the area with COVID-19 hotspots in MPPs (39).
3.4. Practical Actions Against COVID-19 in Slaughterhouses
Using outdoor environment for break times and installation of physical barriers between workers that are close to each other decrease the rate of SARS-CoV-2 spread (Fig. 3). Innovative methods should be applied to educate workers with various native languages in slaughterhouses. Less than half of the employees were educated to use the masks properly and to cover their mouth and nose in Nebraska, the US (46). In addition, employees who were infected by the virus can be provided with medical aids and regular salary to prevent them from working and contaminating other employees. Workers often share their vehicles for the transportation between living areas and slaughterhouses; therefore, the number of passenger per vehicle should be limited, and the volume of public transportation should increase to lessen the spread of the virus. Moreover, frequently touched surfaces including handles, railings, and buttons should be disinfected regularly (15,50,51).
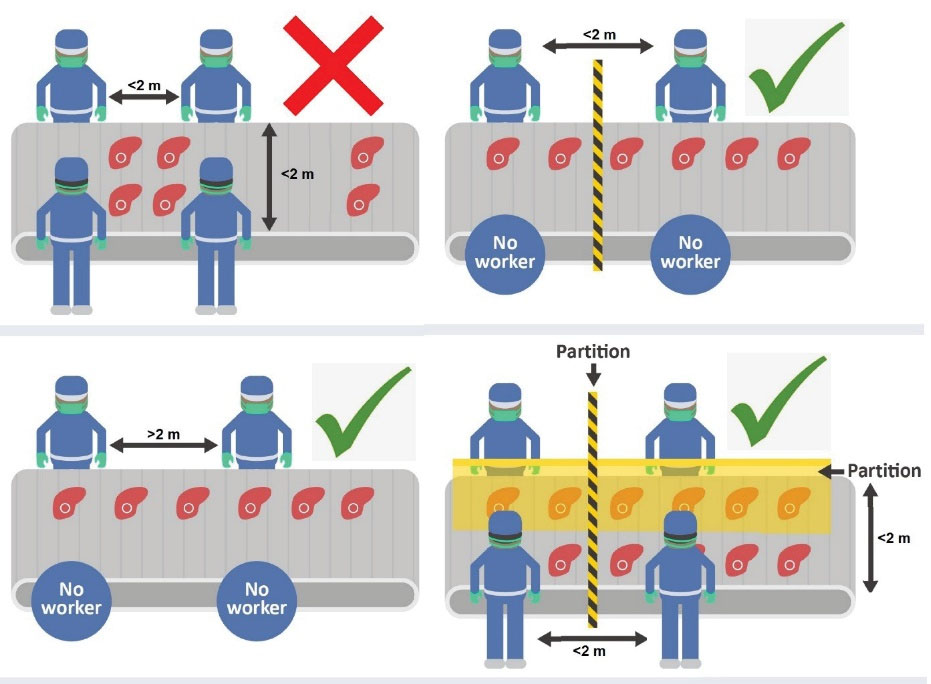
Fig. 3.
Proper and Wrong Standing of Workers Along Production Lines in Meat Processing Plants
.
Proper and Wrong Standing of Workers Along Production Lines in Meat Processing Plants
Since the prevalence of SARS-CoV-2 is higher in large MPPs, an approach for small meat processing facilities and more decentralized plants is required (17). Further, the use of water sluicing, rubber squeegees, and steam hoses is suggested rather than brushes and pressurized hoses to prevent aerosolization. FFP2 and FFP3 masks could also significantly lessen the spread of SARS-CoV-2 among workers of MPPs (18). Additionally, countless and efficient disinfection of hand is recommended during meat processing, manufacturing and marketing (25). Mandatory use of masks and physical barriers caused significant decrease of COVID-19 cases in 8 out of 13 MPPs in Nebraska, the US, during 10 days. Other three MPPs demonstrated non-significant reduction of infected incidence (41). Moreover, well-experienced coordinators are required at each meat processing factory so that all employers and employees can easily raise their COVID-19 questions, and health plans and regulations should be implemented for all staff in MPPs (24).
3.5. Other Engineering Controls
Employees should stand next to each other with a distance of at least two meters in operating areas, especially along production lines. Employers should be prevented from face to face standing of along processing lines. Further, markers can be used to easily remember the previous location of workers, and the direction of air conditioning systems should be designed in such a way that it blows to workers indirectly. In addition, hand sanitizing stations, preferably free touch facilities, with 60% alcohol can be used in different places. Further, the number of in and out shifts and stations as well as the number of break times should be increased in order to decrease the crowded spots during working hours (24).
4. Conclusion
Prevalence of COVID-19 was significantly high in MPPs. The ratio of COVID-19 transmission in workers of MPPs was 24 times higher than the ratio of infected people in the US per whole population. Various factors contributed to this fact such as low indoor temperature, crowded area, wrong standing along with operation lines, contamination of high-touch surfaces, difficult education of ethnic minority employees and migrants, low financial income, large MPPs with 10+ million Ib of meat per month, higher speed of production lines with 175 birds/minute, temporary contract of the employees, and weak performance of some meat processing companies such as National Beef. The practical solutions to this spread were also partitioning the operating areas, using marker for remembering the previous location, using mandatory mask, especially FFP2/3, decentralizing large MPPs, increasing the number of public transportation as well as the number of in and out stations and shifts, employing COVID-19 coordinating experts, indirect blow of air conditioners, and financial aids for ill workers. Therefore, controlling the spread of SARS-CoV-2 is more achievable through the implementation of the suggested solutions.
The main limitation of the current study was that many generalized papers that evaluated COVID-19 spread in MPPs merely based on the title reported general information about the situation of MPPs during COVID-19 outbreak in the context rather than providing specific analysis. Another limitation was related to two Chinese reports that were not considered in this study. Different structure of documents (e.g., newspapers and original papers) was another obstacle for yielding the results.
Acknowledgments
We thank Student Research Committee of Ahvaz Jundishapur University of Medical Sciences for financial supporting of this study (00S102).
Competing Interests
The authors declare that they have no conflict of interests.
Ethical Approval
Ethical approval for this study was obtained under the code of IR.AJUMS.REC.1400.669.
References
- Zhou J, Li C, Zhao G, Chu H, Wang D, Yan HH. Human intestinal tract serves as an alternative infection route for Middle East respiratory syndrome coronavirus. Sci Adv 2017; 3(11):eaao4966. doi: 10.1126/sciadv.aao4966 [Crossref] [ Google Scholar]
- Zhang H, Kang Z, Gong H, Xu D, Wang J, Li Z, et al. The digestive system is a potential route of 2019-nCov infection: a bioinformatics analysis based on single-cell transcriptomes. bioRxiv (Preprint). January 31, 2020. Available from: https://www.biorxiv.org/content/10.1101/2020.01.30.927806v1.
- Letko M, Marzi A, Munster V. Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses. Nat Microbiol 2020; 5(4):562-9. doi: 10.1038/s41564-020-0688-y [Crossref] [ Google Scholar]
- Gu J, Han B, Wang J. COVID-19: gastrointestinal manifestations and potential fecal–oral transmission. Gastroenterology 2020; 158(6):1518-9. doi: 10.1053/j.gastro.2020.02.054 [Crossref] [ Google Scholar]
- Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H. First case of 2019 novel coronavirus in the United States. N Engl J Med 2020; 382(10):929-36. doi: 10.1056/NEJMoa2001191 [Crossref] [ Google Scholar]
- Zhang Y, Chen C, Zhu S, Shu C, Wang D, Song J. Isolation of 2019-nCoV from a stool specimen of a laboratory-confirmed case of the coronavirus disease 2019 (COVID-19). China CDC Wkly 2020; 2(8):123-4. [ Google Scholar]
- Johnson DL, Mead KR, Lynch RA, Hirst DV. Lifting the lid on toilet plume aerosol: a literature review with suggestions for future research. Am J Infect Control 2013; 41(3):254-8. doi: 10.1016/j.ajic.2012.04.330 [Crossref] [ Google Scholar]
- Knowlton SD, Boles CL, Perencevich EN, Diekema DJ, Nonnenmann MW. Bioaerosol concentrations generated from toilet flushing in a hospital-based patient care setting. Antimicrob Resist Infect Control 2018; 7:16. doi: 10.1186/s13756-018-0301-9 [Crossref] [ Google Scholar]
- Verani M, Bigazzi R, Carducci A. Viral contamination of aerosol and surfaces through toilet use in health care and other settings. Am J Infect Control 2014; 42(7):758-62. doi: 10.1016/j.ajic.2014.03.026 [Crossref] [ Google Scholar]
- Guo ZD, Wang ZY, Zhang SF, Li X, Li L, Li C. Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020. Emerg Infect Dis 2020; 26(7):1583-91. doi: 10.3201/eid2607.200885 [Crossref] [ Google Scholar]
- McDermott CV, Alicic RZ, Harden N, Cox EJ, Scanlan JM. Put a lid on it: are faecal bio-aerosols a route of transmission for SARS-CoV-2?. J Hosp Infect 2020; 105(3):397-8. doi: 10.1016/j.jhin.2020.04.024 [Crossref] [ Google Scholar]
- Mao K, Zhang H, Yang Z. Can a paper-based device trace COVID-19 sources with wastewater-based epidemiology?. Environ Sci Technol 2020; 54(7):3733-5. doi: 10.1021/acs.est.0c01174 [Crossref] [ Google Scholar]
- Durai P, Batool M, Shah M, Choi S. Middle East respiratory syndrome coronavirus: transmission, virology and therapeutic targeting to aid in outbreak control. Exp Mol Med 2015; 47(8):e181. doi: 10.1038/emm.2015.76 [Crossref] [ Google Scholar]
- Cauchemez S, Nouvellet P, Cori A, Jombart T, Garske T, Clapham H. Unraveling the drivers of MERS-CoV transmission. Proc Natl Acad Sci U S A 2016; 113(32):9081-6. doi: 10.1073/pnas.1519235113 [Crossref] [ Google Scholar]
- Waltenburg MA, Victoroff T, Rose CE, Butterfield M, Jervis RH, Fedak KM. Update: COVID-19 among workers in meat and poultry processing facilities - United States, April-May 2020. MMWR Morb Mortal Wkly Rep 2020; 69(27):887-92. doi: 10.15585/mmwr.mm6927e2 [Crossref] [ Google Scholar]
- Guenther T, Czech-Sioli M, Indenbirken D, Robitailles A, Tenhaken P, Exner M, et al. Investigation of a superspreading event preceding the largest meat processing plant-related SARS-Coronavirus 2 outbreak in Germany. 2020. Available from: https://ssrn.com/abstract=3654517.
- Taylor CA, Boulos C, Almond D. Livestock plants and COVID-19 transmission. Proc Natl Acad Sci U S A 2020; 117(50):31706-15. doi: 10.1073/pnas.2010115117 [Crossref] [ Google Scholar]
- Donaldson AI. Aerosols in meat plants as possible cause of COVID-19 spread. Vet Rec 2020; 187(1):34-5. doi: 10.1136/vr.m2702 [Crossref] [ Google Scholar]
- Dyal JW, Grant MP, Broadwater K, Bjork A, Waltenburg MA, Gibbins JD. COVID-19 among workers in meat and poultry processing facilities - 19 states, April 2020. MMWR Morb Mortal Wkly Rep 2020; 69(18):557-61. doi: 10.15585/mmwr.mm6918e3 [Crossref] [ Google Scholar]
- Matson MJ, Yinda CK, Seifert SN, Bushmaker T, Fischer RJ, van Doremalen N. Effect of environmental conditions on SARS-CoV-2 stability in human nasal mucus and sputum. Emerg Infect Dis 2020; 26(9):2276-8. doi: 10.3201/eid2609.202267 [Crossref] [ Google Scholar]
- Notari A, Torrieri G. COVID-19 transmission risk factors. medRxiv (Preprint). May 17, 2021 (Cited 2020 November 3). Available from: https://www.medrxiv.org/content/10.1101/2020.05.08.20095083v2.
- Notari A. Temperature dependence of COVID-19 transmission. medRxiv (Preprint). April 24, 2020 (Cited 2020 November 3). Available from: https://www.medrxiv.org/content/10.1101/2020.03.26.20044529v3.
- Food and Environment Reporting Network (FERN). Mapping COVID-19 Outbreaks in the Food System. 2020. Available from: https://thefern.org/2020/04/mapping-covid-19-inmeat-and-food-processing-plants. Accessed October 17, 2020.
- CDC, OSHA. Guidance on Mitigating and Preventing the Spread of COVID-19 in the Workplace. Available from: https://www.cdc.gov/coronavirus/2019-ncov/community/organizations/meat-poultry-processing-workers-employers.html.
- WHO. COVID-19 and Food Safety: Guidance for Food Businesses. 2020. Available from: https://www.who.int/publications-detail/covid-19-and-food-safetyguidance-for-food-businesses.
- Ong SWX, Tan YK, Chia PY, Lee TH, Ng OT, Wong MSY. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA 2020; 323(16):1610-2. doi: 10.1001/jama.2020.3227 [Crossref] [ Google Scholar]
- World Health Organization (WHO). First Data on Stability and Resistance of SARS Coronavirus Compiled by Members of WHO Laboratory Network. WHO; 2020. Available from: https://www.who.int/csr/sars/survival_2003_05_04/en/. Accessed July 16, 2020.
- Chin AWH, Chu JTS, Perera MRA, Hui KPY, Yen HL, Chan MCW. Stability of SARS-CoV-2 in different environmental conditions. Lancet Microbe 2020; 1(1):e10. doi: 10.1016/s2666-5247(20)30003-3 [Crossref] [ Google Scholar]
- van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 2020; 382(16):1564-7. doi: 10.1056/NEJMc2004973 [Crossref] [ Google Scholar]
- Aboubakr HA, Sharafeldin TA, Goyal SM. Stability of SARS-CoV-2 and other coronaviruses in the environment and on common touch surfaces and the influence of climatic conditions: a review. Transbound Emerg Dis 2021; 68(2):296-312. doi: 10.1111/tbed.13707 [Crossref] [ Google Scholar]
- Bai Y, Yao L, Wei T, Tian F, Jin DY, Chen L. Presumed asymptomatic carrier transmission of COVID-19. JAMA 2020; 323(14):1406-7. doi: 10.1001/jama.2020.2565 [Crossref] [ Google Scholar]
- Chen YC, Huang LM, Chan CC, Su CP, Chang SC, Chang YY. SARS in hospital emergency room. Emerg Infect Dis 2004; 10(5):782-8. doi: 10.3201/eid1005.030579 [Crossref] [ Google Scholar]
- Bundesinstitut für Risikobewertung (BfR). Can SARS-CoV-2 Be Transmitted Via Food And Objects? 2020. Available from: https://www.bfr.bund.de/en/can_the_new_type_of_coronavirus_be_transmitted_via_food_and_objects_-244090.html.
- European Food Safety Authority (EFSA). Coronavirus: No Evidence That Food is a Source or Transmission Route. 2020. Available from: https://www.efsa.europa.eu/en/news/coronavirus-no-evidence-food-source-or-transmission-route.
- Xiaodong W. No Import Food Found with Virus After Cluster Infections. China Daily; 2020.
- Liu C. Beijing Supermarkets Stop Selling Salmon After Wholesalers Test Positive for Coronavirus. Global Times; 2020.
- Over 450 Covid-19 cases reported at food factories in England and Wales. https://www.theguardian.com/uk-news/2020/jun/25/over-450-covid-19-cases-reported-at-food-factories-in-england-and-wales.
- Society of Occupational Medicine (SOM). Occupational Health: The Global Value and Evidence. 2018. Available from: www.som.org.uk/sites/som.org.uk/files/Occupational_Health_the_Global_Value_and_Evidence_April_2018.pdf.
- de Rooij MMT, Sikkema RS, Bouwknegt M, de Geus Y, Stanoeva KR, Nieuwenweg S, et al. Potential environmental transmission routes of SARS-CoV-2 inside a large meat processing plant experiencing COVID-19 clusters. medRxiv (Preprint). June 25, 2021. Available from: https://www.medrxiv.org/content/10.1101/2021.06.20.21259212v1.
- Pokora R, Kutschbach S, Weigl M, Braun D, Epple A, Lorenz E. Investigation of superspreading COVID-19 outbreak events in meat and poultry processing plants in Germany: a cross-sectional study. PLoS One 2021; 16(6):e0242456. doi: 10.1371/journal.pone.0242456 [Crossref] [ Google Scholar]
- Herstein JJ, Degarege A, Stover D, Austin C, Schwedhelm MM, Lawler JV. Characteristics of SARS-CoV-2 transmission among meat processing workers in Nebraska, USA, and effectiveness of risk mitigation measures. Emerg Infect Dis 2021; 27(4):1032-8. doi: 10.3201/eid2704.204800 [Crossref] [ Google Scholar]
- Baboli Z, Neisi N, Babaei AA, Ahmadi M, Sorooshian A, Tahmasebi Birgani Y. On the airborne transmission of SARS-CoV-2 and relationship with indoor conditions at a hospital. Atmos Environ (1994) 2021; 261:118563. doi: 10.1016/j.atmosenv.2021.118563 [Crossref] [ Google Scholar]
- United States Coronavirus Cases. Available from: https://www.worldometers.info/coronavirus/country/us/#graph-cases-daily.
- United States Population 1950-2022. Available from: https://www.macrotrends.net/countries/USA/unitedstates/population#:~:text=The%20current%20population%20of%20U.S.,a%200.58%25%20increase%20from%202020.
- Durand-Moreau Q, Adisesh A, Mackenzie C, Bowley J, Straube S, Chan XH, et al. COVID-19 in Meat and Poultry Facilities: A Rapid Review and Lay Media Analysis. Centre for Evidence-Based Medicine; 2020.
- University of Nebraska Medical Center (UNMC). Concerns and Perceptions of COVID-19 Among Meatpacking Plant Workers in Nebraska. 2020. Available from: https://www.unmc.edu/healthsecurity/covid-19/meatprocessing/UNMCMeatpacking-study-results-1-page-bilingual.pdf. Accessed October 11, 2020.
- Centers for Disease Control and Prevention (CDC). How COVID-19 Spreads. 2020. Available from: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fprepare%2Ftransmission.html.
- Fernstrom A, Goldblatt M. Aerobiology and its role in the transmission of infectious diseases. J Pathog 2013; 2013:493960. doi: 10.1155/2013/493960 [Crossref] [ Google Scholar]
- Pittet D, Allegranzi B, Sax H, Dharan S, Pessoa-Silva CL, Donaldson L. Evidence-based model for hand transmission during patient care and the role of improved practices. Lancet Infect Dis 2006; 6(10):641-52. doi: 10.1016/s1473-3099(06)70600-4 [Crossref] [ Google Scholar]
- Rahmani AR, Azarian G, Poormohammadi A. Health impacts of long-term exposure to disinfectants during SARS-Cov-2 pandemic. Avicenna J Environ Health Eng 2020; 7(1):53-4. doi: 10.34172/ajehe.2020.08 [Crossref] [ Google Scholar]
- Mahmudiono T, Ramaiah P, Maleki H, Doewes RI, Shalaby MN, Alsaikhan F, et al. Evaluation of the impact of different disinfectants on new coronavirus and human health. Rev Environ Health. 2022. 10.1515/reveh-2022-0051.