Avicenna J Environ Health Eng. 7(2):109-117.
doi: 10.34172/ajehe.2020.16
Systematic Review
Transmission Routes of COVID-19 Through Air, Water and Wastewater: A Systematic Review
Nematollah Jaafarzadeh 1  , Sahand Jorfi 1, Zeinab Ghaedrahmat 2, 3, Halime Almasi 2, 3, *
, Sahand Jorfi 1, Zeinab Ghaedrahmat 2, 3, Halime Almasi 2, 3, *  , Amir Zahedi 2, 3, *
, Amir Zahedi 2, 3, *
Author information:
1Environmental Technologies Research Center, Department of Environmental Health Engineering, Ahvaz Jundishapur University of Medical Sciences. Ahvaz, Iran
2Department of Environmental Health Engineering, Shoushtar Faculty of Medical Sciences, Shoushtar, Iran
3Student Researcher Committee, Shoushtar Faculty of Medical Sciences, Shoushtar, Iran
Abstract
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). In this systematic review, five databases were searched (Scopus, PubMed-/Medline, Cochrane library, Embase, and Web of Science) for publications between 2019 to 12 February 2021. From 575 articles identified, seven papers were selected for inclusion. In the present paper, corona transmission routes from three environments of water, wastewater and air were considered. The most important transmission route of COVID-19 is through the air, which takes place from the following two routes: respiration and contact. Respiratory drops are caused by coughing and sneezing. Anyone who comes in close contact with someone having COVID-19 symptoms (sneezing, coughing, etc.) is potentially at risk for droplets. In this paper, corona transmission pathways from water, wastewater, and air in three environments were investigated. The results showed that the virus is transmitted through the air and its transmission through water and wastewater has not been proven. While the virus may survive in drinking water, there is no evidence that human coronavirus is present in surface and groundwater sources, or transmitted through contaminated drinking water. There is also no evidence of SARS-CoV-2 transmission through the sewage system, with or without wastewater treatment. Detection of this virus is very effective in determining the necessary and timely strategies to prevent further transmission of virus, and help to break the chain of COVID-19 transmission through water and wastewater.
Keywords: Corona virus, COVID-19, Air, Water, Wastewater
Copyright and License Information
© 2020 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
1. Introduction
Viruses are the smallest (with exceptions), most abundant, and most diversified biological organisms that can infect any forms of plant, bacterial, and animal life (with exceptions). The viral infection is a complex multi-step phenomenon in which the virus attaches to the host cells. Interactions between the virus and host cell membrane receptors determine the degree of virus and pathogens specialization (1). Viral tissue tropism (cell surface receptors that determine which viruses can infect the cell) and the host spectrum are enhanced by multiple infection mechanisms (specificity switching) and host coatings (1). Due to this self-engineering ability, the spread of the virus is inevitably uncontrollable. The situation becomes more serious when these smallest biological organisms make their way quickly through obstacles between hosts. This subject has confused medical research communities (1). Coronaviruses are a large family of viruses and subfamilies of Nidovirales, which include the families Coronaviridae, Arteriviridae, and Roniviridae. They are considered as an agent of the common cold virus to more severe diseases such as severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS), and COVID-19 (coronavirus disease 2019) (2). Coronaviruses have two different types of surface proteins, and get their name from this appearance. The coronavirus family is genotypically and serologically divided into alpha, beta, gamma, and delta. Approximately 30 species of coronaviruses have been identified in humans, mammals, and birds. Human coronaviruses are caused by alpha and beta (3). COVID-19 is the third known animal coronavirus disease after SARS and MERS, both of which belong to betacoronavirus group (4). In 2019 in Wuhan, a new coronavirus called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was identified that had caused respiratory illness. This new virus is currently spreading rapidly all over the world and, therefore, it is important for specialists to identify its features and characteristics in order to protect health workers and employees against it. The symptoms of the new virus are different from other coronavirus diseases (1). Coronavirus (CoV) is a large family of RNA-positive single-stranded RNA viruses that causes coronavirus 2019, which is common among various animal species such as camels, cows, cats, and bats. Virus genome sizes are between 27 to 32 kb, which show a high degree of adaptation of genome plasticity and diversity with CoV (3). COVID-19 has a length of 120-160 nm, adorned with apical or petiole-shaped appendages (papilloma or thorns), which can be seen in the electron micrograph of the sun-like crown. Therefore, members of this family are known as coronaviruses. COVID-19 is the newest member of Coronaviridae, which has the highest number of deaths compared to other families (3). Early investigations of pneumonia cases of coronavirus in epidemiological studies have shown that many cases have been exposed to the Huanan (Huanan seafood market) in Wuhan, China. Report of the World Health Organization (WHO) also states that the new coronavirus has been identified in environmental samples collected from the Huanan seafood market, but it is not clear yet what specific species of animals carry the new coronavirus (4-6).
The most common symptoms of COVID-19 include fever, fatigue, and dry cough. Some patients may have pain, nasal congestion, runny nose, sore throat, or diarrhea. These symptoms are usually mild and begin gradually. Some people become infected but have no symptoms and no discomfort (7). As a general principle, respiratory viruses are mainly transmitted through tiny droplets caused by coughing or sneezing or touching infected objects. The mortality rate from this virus is reported to be about 2%. Guan et al reported a 1.4% mortality rate among 1099 patients with laboratory-confirmed COVID-19 (4).
Currently, the origin, susceptibility population, and sources of infection are known. However, routes of transmission, which are key steps in controlling the spread of the disease, have not yet been fully described. Here we focused on the possible transmission paths that have been studied in the SARS-CoV-2 epidemic (8). The distribution of the viral receptor can determine pathogenic mechanisms, clinical manifestations, and routes of modern coronavirus transmission (9,10). Corona is a highly contagious virus, and since it has been originated from china through human-to-human transmission, four known pathways have been considered for spreading the virus from an infected person to a healthy one, including 1) Polluted Air 2) Contaminate food 3) Transmission through wastewater 4) Transmission through drinking water. Coronavirus transmission, like colds and flu, is transmitted through the patient’s airways. COVID-19, similar to SARS and MERS, is spread mainly through high-respiratory tract infections, and droplets transmission is usually considered as the main route of the virus (8).
In airborne diseases, when an infected person coughs, sneezes, talks, or spends a lot of time close to others, the virus is released by transmitted droplets (7,11). Normally, droplets do not travel more than six feet (about two meters) and do not stay in the air (8). Microbes are transmitted by people using cough, sneeze, and inhaled droplet. In direct contact, when a person is ill, the virus is present on the person’s hand and can be transmitted to others through contact if the person has already touched his/her mucous membranes of the eye, nose, or mouth (7,11).
1) Indirect contact (deposited on objects) with polluted tools and equipment: Previous studies have shown that different human viruses, such as SARS-CoV and MERS-CoV, can survive on inanimate surfaces for different periods. An infection can also occur if the surface is polluted and then the eyes, nose, or mouth are touched, but it does not seem to be the main route of the virus spread (8). In indirect contact, transmission of the virus occurs through objects or surfaces (e.g., door handles, keyboards, telephones)together with sneezing or coughing, or by a sick person holding the virus on their hands and then touch the objects and surfaces. In the case of swimming pools, the amount of chlorine in the pool water is sufficient to inactivate” the Covid-19, although physical contact during bathing can lead to transmission. 2) Contaminated food (7,11). 3) Transmission through wastewater, 4) Transmission through drinking water (12). So far, the outline of transmission routes of SARS-CoV-2 has not been provided. More efforts should be made to provide a complete picture of the transition, so that public health measures can be taken in a timely manner by the government to prevent further spread. Extensive research on COVID-19 is needed to fully clarify the transmission routes and its pathogenic mechanisms, which can be effective in developing common preventive and treatment methods.
2. Methods
2.1. Information Sources and Search Strategy
To find English articles in databases, namely PubMed/Medline, Scopus, ISI Web of Science, Cochrane library, and Embase, certain keywords including COVID-19, transmission (Mesh), SARS-Cov2(Mesh), OR coronavirus(Mesh) AND airborne(Mesh) AND transmission (Mesh), wastewater (Mesh), and water (Mesh) were used according to (Mesh). Articles were searched from 2019 to Feb 2021. The search strategy was carried out based on the PRISMA flow diagram (Fig. 1). The purpose of the present study was to investigate the transmission routes of coronavirus from different pathways such as airways, and contaminated surfaces. Independently, databases were searched based on the above materials to find potentially relevant studies. Full-text articles published in English and available online – either for free or via an institution’s subscription, were selected.
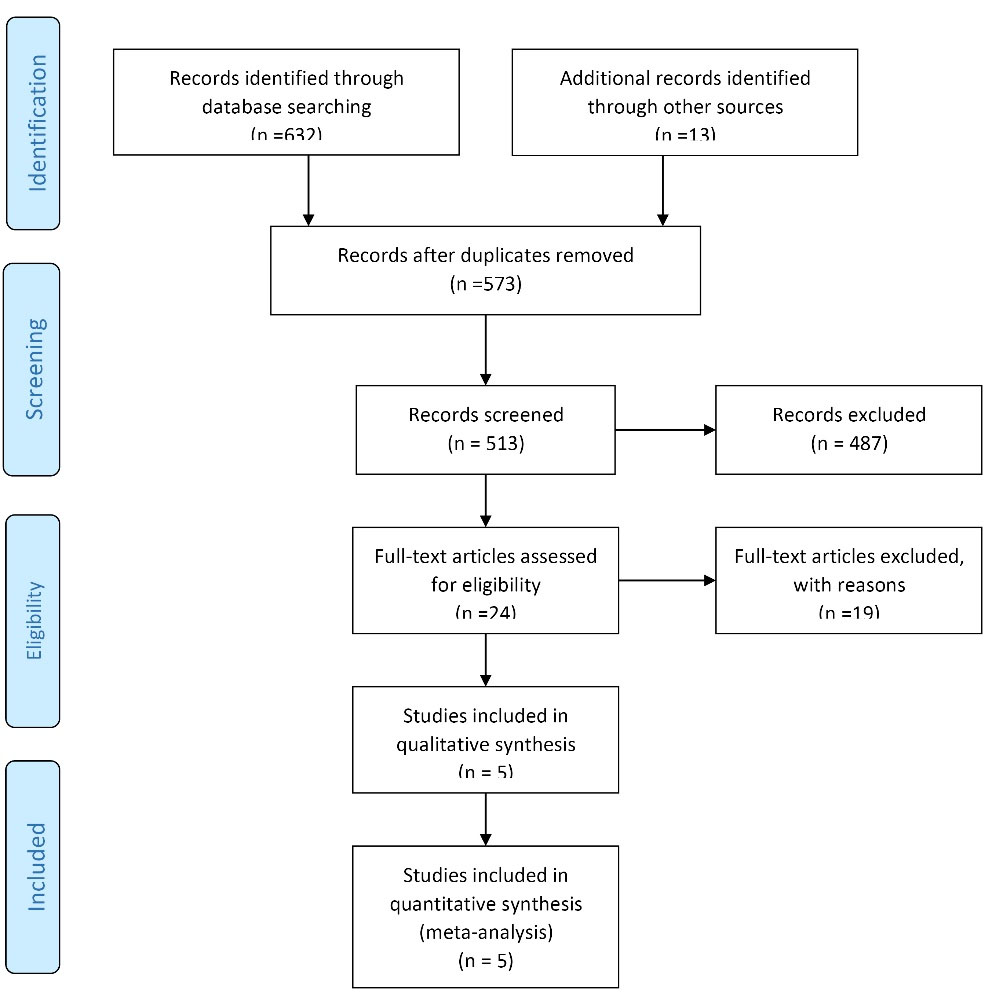
Figure 1.
Flow Diagram of Study Searches.
.
Flow Diagram of Study Searches.
2.2. Inclusion/Exclusion Criteria for The Included Studies
All or part of the PICO elements expected to be present in the articles were found to be used in this review design (study population, intervention). Inclusion criteria in the present systematic study included all studies published in English, and studies examining the pathways of coronavirus transmission. Other published papers in other languages were excluded.
Patient Problem (or Population): Studies in which the study population included all infected individuals with coronavirus.
Intervention: Corona virus.
Comparison: Studies that examined the relationship between the coronavirus and its transmission pathways.
Outcome: Studies that examined the transmission pathways of coronavirus.
Exclusion criteria: review articles, duplicated papers, and language.
3. Results and Discussion
3.1. Study Characteristics
To carry out this study, 645 studies were selected and 77 citations were used. Then, a summary of 573 unique studies (309 from PubMed, 63 EMBASE, 164 from SCOPUS, 2 from Cochran library, and 107 from other sources) was examined. Articles selected for analysis had the following features: All or part of the PICO (population, intervention, comparison, and outcomes) components that were expected to be found in the articles were used in this review, and full-text available. Due to the heterogeneity of the collected data from the results of the studies, meta-analysis was not performed. The general characteristics of the literature review were presented in Table 1 (13-17).
Table 1.
Summary of Studies
|
Author
|
Specific or for Similar Viruses
|
Type of Transmission
|
Country/Region
|
| Jiang et al |
Specific (for COVID-19) |
Airborne and contact direct |
China |
| Faridi et al |
Specific (for COVID-19) |
Airborne |
Iran |
| Morawska et al |
Specific (for COVID-19) |
Airborne |
Australia |
| Sun et al |
Specific (for COVID-19) |
Indirect contact |
China |
| Zhang et al |
Specific (for COVID-19) |
Airborne and contact direct |
China |
| Wang et al |
Specific (for COVID-19) |
Indirect contact |
China |
3.2 Airborne Transmission
In a report on January 30, 2020, the WHO stated that the coronavirus outbreak was the sixth leading cause of worldwide public health emergency and, therefore, was a threat for all countries (18). On February 11, 2020, this organization officially chose the name COVID-19 for new coronavirus, and on the same day, International Committee on Taxonomy of Viruses (ICTV) for virus classification changed the name of the virus from nCoV-2019 to SARS CoV-2 (18).
Acute lower respiratory tract infections – including pneumonia, are the most common cause of the world’s total deaths. The virus is transmitted to the environment through the respiratory tract and spreads to other people. Respiratory infections can be an asymptomatic disease and, therefore, create a serious threat to human health and his immune system (19,20). Airborne spread of infectious agents depends directly on airborne pathways and indirectly on droplet-borne and fomite pathways (21). One transmission route that is mentioned only in passing, or not at all, is the transport of virus-laden particles in the air (22). It has been accepted that the droplet transmission is the main route of the virus spread. The respiratory viruses can be transmitted through the air with droplets or aerosol (8). The length of time for droplet-nuclei is determined by their size. The size of the droplet nuclei is more important for entering the respiratory tract because some of the particles that are inhaled during respiration belong to this category. The usual accepted cutting size between the large droplets and small aerosol is 5 µm, although this rate varies significantly between studies up to about 12 µm (16). Droplets larger than 5-10µ are called respiratory droplets and those with less than 5µ are referred to as droplet nuclei. Particles larger than 5µ in diameter – remaining only shortly in the air (<17 minutes) and dispersing over short distances (<1 m) – are held in place by centrifugal force in the upper respiratory tract (nasal cavity), while particles smaller than 5µ – Aerosols, droplet nuclei (<5 mm) remaining in the air for an almost infinite amount of time and dispersing over long distances (>1 m) – are deposited in the alveoli of the lungs, which is of great importance in lung infection (22,23).
Droplets from coughing, sneezing, and talking do not stay suspended in the air and move less than 1 meter before settling on the mucous membranes of nearby contacts or environmental surfaces. If there are certain amounts of pathogens in the droplets, they may be inhaled and spread by others. Sneeze droplets are spread more than those of coughs (16). Aerosols have slow-velocity, so they stay suspended in the air for longer periods and can travel longer distances (13,19). The chance of spreading the infection is determined by airborne droplets when talking, coughing and sneezing, and it depends on how long the droplets stay in the air, which is largely determined by their size. When a person sneezes, up to 40 000 droplets are expelled at a velocity of 100 meters per second and in a cough, this amount decreases to about 3000 droplets (21). Droplets larger than 100 µ in diameter fall on the ground in about 1 or 2 seconds, while droplets smaller than 100µ evaporate and turn to droplet-nuclei form before falling on the ground, and may remain airborne for some hours or even days. Droplets of saliva disappear a little slower, but due to the predominant influence of size are likely to be a function of the generation process and the environmental conditions. (22).
The transmission route of COVID-19 is complex and depends not only on environmental factors (e.g., humidity and temperature), but also on host factors such as the receptor distribution using respiratory tract. The fact is that different agents affect the routes of transmission of the respiratory viruses, which are very difficult to consider experimentally (19). WHO reported that viral infections can be transmitted remotely by suspended particles (such as airborne infections) to indoor environments and can lead to many infections in a short period. Due to the many similarities between SARS and COVID-19 viruses, probably SARS-CoV-2 virus will also be spread through the air (16) (Fig. 2).
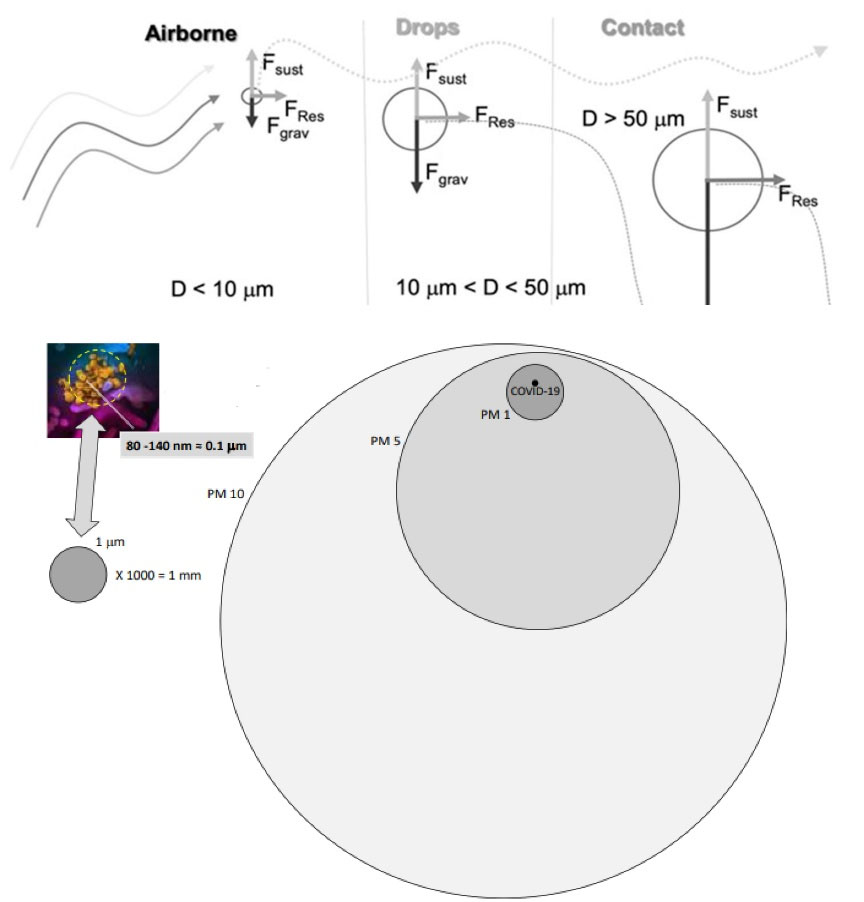
Figure 2.
Typical Particle Trajectory for Air Particles Relative to Their Dimension (24).
.
Typical Particle Trajectory for Air Particles Relative to Their Dimension (24).
3.2.1 Direct Contact
Transmission routs of the new coronavirus in direct contact include an infected person, sneezing, coughing, breathing, and airborne particles. Some studies have shown that normal breathing and speech scatter significant amounts of aerosol particles in the environment. Expiratory particles are usually about 1 micron in size and cannot be seen with the naked eye. These particles are sufficiently large to transmit viruses such as COVID-19, and are also within a range that can be easily inhaled by a susceptible person’s respiratory tract (25). Airborne transmission is the process by which airborne droplets are released, and people who inhale these environmental aerosols become infected. Several infectious diseases are transmitted by droplets. The transmission of infectious diseases depends on the size of the cough or sneezing droplets (26). Therefore, determining the size of the respiratory droplets is important to prevent the spread of the disease. Studies have shown that virus transmission is possible through direct contact with a person who has symptoms, as well as through respiratory droplets and handshakes. Infected respiratory droplets are released into the environment through sneezing or coughing of an infected person and are deposited on the mouth or nose of people close to the patient, and then transferred into their lungs (8).
COVID-19 has been also found in patients’ saliva. Saliva can be secreted by coughing; and even during normal breathing, the respiratory droplets of the influenza virus have also been found. In patients with symptoms or when there is no cough, COVID-19 can still be transmitted directly or indirectly through saliva. Saliva samples include not only saliva secreted from the salivary glands, but also saliva produced by nasopharyngeal or lung secretions. Isolated sequence analysis of COVID-19 and SARS-CoV use the same angiotensin-converting enzyme (ACE2) to invade the cells. German researchers have isolated 2019-nCoV from the soft tissue of the mild patients’ nose and confirmed that the virus can spread to the nasal cavity and throat, and can be transmitted by asymptomatic or mild patients (17,27). Previous studies have shown that the size of respiratory droplets in healthy individuals is 1.6, 2.5 and 145 µm during speech, and 1.6, 1.7 and 123 µm during cough. Therefore, these particles are transferred over time with the flow of the air. The characteristics of the produced respiratory droplets are related to human health conditions. For example, studies on influenza patients and upper respiratory tract infections have shown reduction in produced aerosol particles when people recovered from illness (28).
The number of infectious agents released into the environment by an infected person depends on the location of the respiratory tract where they originate from. Pathogenic microorganisms are generally present in some areas, especially in the tonsils and larynx, and are found rarely in front of the mouth (21). Three modes are recommended for droplet size :1) the bronchiolar fluid film burst including produced droplets during normal breathing with a diameter of less than or equal to 1 μm micrometer. 2) the laryngeal mode, most active during voicing and coughing (d ≥ 1 μm); and the oral cavity mode, active during speech and coughing, producing droplets ≥100 μm. Basically, the oral cavity has droplets with ≥20 μm. The produced droplets of the trachea during coughing may not be spread into the environment because they easily settle in the head airways.
The size of the COVID-19 virus is 70-90 nm. If the size of a respiratory droplet is considered 0.09 µm and it contains a single COVID-19 (maximum size file), it is estimated that the 1-mm-size droplet will contain 10E12 viruses. That is to say, it can be considered that 100% of the respiratory droplets fluid are full of the virus (28). Another study reported that distances of horizontal transmission of droplets was greater than 2 meters (≈6 feet). The maximum distance based on a few studies has reached 8 meters (≈26 feet). The horizontal distance of droplets depends on different variables such as viscoelasticity of the expiration fluid, type of ventilation, the velocity of expiration, rate of evaporation, and the dynamics of turbulent cloud generated during exhalations, sneezing, or coughing. Considering the size of droplets (less than 20 µm in diameter) and body temperature (the main agent in the spread of the virus), local airflow raises the droplets in the upward breathing area (29) (Fig. 3).
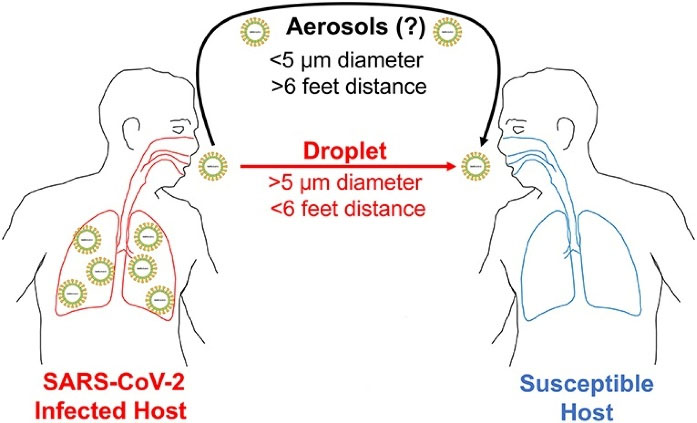
Figure 3.
COVID-19 Potential Modes of Transmission (30).
.
COVID-19 Potential Modes of Transmission (30).
3.2.2 Indirect Contact
In direct or indirect transmission, a susceptible person needs to physically touch a virus-contaminated hand (person-to-person) and fomite (object), respectively. Although airborne transmission needs no physical contact between infected and susceptible individuals, in both direct and indirect contact aerosol transmission is considered as an important main route of transmission (31). The carrier of expiratory droplets can be described in two steps: 1) Exhale with the main expiratory stream, 2) The secondary diffusion with airflow through the room. The velocity rate in buildings is generally less than 0.25 m/s for thermal comfort. Typical airflows are turbulent and depend on various parameters including body thermal plumes, and human conversational behavior and activities. The size of the droplets affects their dispersion and sedimentation on the surfaces and the survival of microorganisms (21).
Saliva drops caused by sneezing or coughing only travel a short distance in the air, after which they sit on people’s bodies or surfaces; so, it is recommended that the hands be constantly washed (due to contact with surfaces) and people avoid hitting their faces (17). Other ways to transmit this virus are spreading from contaminated surfaces or objects. It may be possible for a person to receive COVID-19 by touching a surface or object on which the virus is present and then touching their mouth, nose, or even their eyes, but it has not been verified to be the main route of virus spread. Previous studies have shown that different human viruses such as SARS-CoV and MERS-CoV can survive on inanimate surfaces for different periods (8). Coronavirus transmission, like colds and flu, is done through the patient’s airways. In indirect contact, the virus is transmitted to people when the objects or surfaces (e.g., door handles, keyboards, telephones, etc.) are first contaminated via sneezing or coughing, or a sick person carrying the virus on his hands, and then are touched by them. Transmission can also be traced mainly to direct or indirect physical contact. In the case of swimming pools, the amount of chlorine in the pool water is sufficient to inactivate viruses, including COVID-19, although physical contact during bathing can lead to transmission (8).
Tear secretions, just like nasal mucosa, can transmit the COVID-19. Eye conjunctivitis occurs due to a quick exposure to infectious droplets and fomites in close contact with infected patients or contaminated hands. For this reason, conjunctivitis is likely to be one of the main causes of human CoVs, and tear and ocular secretions may contain the virus, thereby transmitting the viral infection. However, there are still disagreements about the role of the eye in the transmission routes (15). Anatomically, the mucosa of the ocular surface (conjunctiva and cornea) and upper respiratory tract is connected by the nasolacrimal duct. Corona is a virus that attaches to mucosal cells in the eyes, nose, and mouth and enters the body through airway cells. It is produced and distributed inside these cells and penetrates other cells. When a person speaks, coughs, and sneezes, the virus settles in small droplets in the air and spreads on the surface, and can be transmitted to other people. Symptoms include cough, sore throat, and shortness of breath, sometimes with severe symptoms (15).
ACE is the entry receptor of 2019-nCoV, SARS-CoV and HCoV-NL63, which presents on human lung alveolar epithelial cells, human conjunctival, and corneal epithelial cells. This receptor is much less observed in the human eye compared to his lung tissues and kidneys. Improper habits such as rubbing and scratching the eyes or even rubbing the eyelids are habits that can create a direct way for COVID-19 transmission (15). It is suspected that eyes play three important roles in corona transmission. Firstly, it is the main goal for human COVs. Secondly, the conjunctiva is probably the gateway to human corona of respiratory infections. Thirdly, tears and conjunctival secretions may develop a way for transmitting human COVs. The eye is rarely involved in SARS-CoV, MERS-CoV, and 2019-nCoV infections. Conjunctivitis has been reported in only five cases as the cause of COVID-19 transmission, which indicates that the eye is not a reference organ for human COV infection. It is not the main way for COV to enter the human’s respiratory tract (15). Hence, the conjunctiva is postulated to be an important portal of entry for Human CoVs, while tear and ocular secretions may contain the virus and spread viral infection (15).
Human coronaviruses such as SARS, MERS, and human endemic coronavirus (HCoV-229E) can survive on surfaces such as metal, glass, or plastic for several days. It is not clear how long the 19-COVID-19 virus can survive on the surface, but it seems that the virus acts like other viruses in the corona family. Therefore, contaminated surfaces that are in contact with the hygienic environment can be a potential source of coronavirus transmission. Processes in which tiny droplets or aerosols are produced from infected patients can lead to contamination of all surfaces. Moreover, researches have shown that human endemic corona remains contagious at room temperature for 2 hours to 9 days and is 50% more resistant to relative humidity. Thus keeping the surface clean and dry helps reduce the durability of the new corona virus (14,32) (Fig. 4).
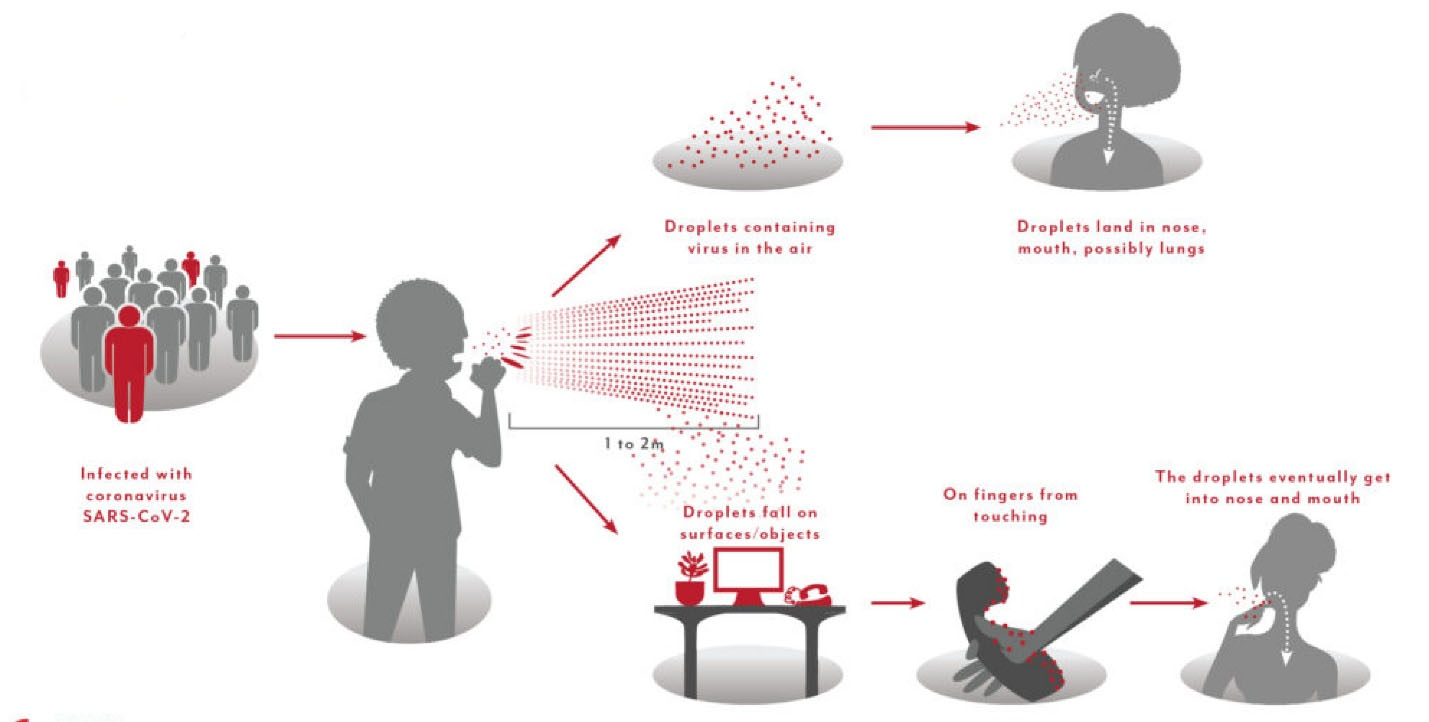
Figure 4.
Indirect Transmissionof Coronavirus.
.
Indirect Transmissionof Coronavirus.
3.3. Transmission of COVID-19 Through Wastewater
What appears to be the corona transmission through wastewater is speculative, and requires further researches. It is generally stated that the viral respiratory infections are caused by direct contact, such as contact with an infected person or surfaces, objects and equipment that the sick person has already been in contact with. It is also believed that saliva droplets or droplets from the sneeze that have entered the environment by an infected person carrying the virus for several days can be another route for transmission (14,33). Although the virus is spread mainly through the respiratory particles of the patient and through contaminated hand contact with the mouth, nose and eyes eventually causing respiratory infection in humans and increasing the mortality rate caused by it, this virus enters in the sewer network through the respiratory secretion, excreta of patients and wastewater from washing, and is likely to be spread through wastewater and surface water, which receive untreated sewage wastewater (34). Frrtthermore, due to the increase in weather temperature in recent days, most patients with suspected coronation go to hospitals with gastrointestinal symptoms, which doubles the possibility of transmitting the virus through food and drinks especially water (9,13,14). According to the Centers for Disease Control and Prevention (CDC), the virus “has been found in untreated wastewater,” but “the researchers do not know whether this virus can cause disease if a person is exposed to untreated wastewater or sewerage systems”, and “there is no evidence of the date that this has occurred (35).
3.4. Transmission of COVID-19 Through Water
Most researchers believe that most public drinking water sources are safe, and this belief could lead to sewage being placed in private wells or public water sources in a limited number of cities whose water sources are not disinfected with chlorine (34). However, these researchers have previously stated that they do not expect to have a problem with drinking water where residents are connected to municipal sewage and water treatment systems. There have been studies (e.g., concerning SARS) concluding that “coronaviruses can remain infectious for long periods in water and pasteurized settled sewage, suggesting contaminated water is a potential vehicle for human exposure if aerosols are generated.” However, it is important to note that these studies failed to find that a person could be infected under normal conditions when exposed to water. The CDC’s position remains the same as it states that COVID-19 has not been detected in drinking water, and conventional water treatment methods using filtration and disinfection (like those found in most municipal drinking water systems) (36) should be effective in removing or inactivating the virus that causes COVID-19 (35).
4. Limitations
Given the fact that the overall design of COVID-19 transmission routes has not been developed yet, we focused on the possible transmission routes that had recently been explored in the recent epidemic and other corona epidemics. Unpublished data were also excluded.
5. Conclusion
This systematic review provided information about transmission routes of COVID-19 in the world. We collected the accessible scientific documents from around the world to show transmission routes of coronavirus. The present study provided evidence of the deadly effects brought about by COVID-19 through direct and indirect contact, airborne spread, and other pathways in the environment. When an infected person coughs or sneezes, respiratory droplets and aerosols, in particular, are important in transmission of this disease. Therefore, people who are in direct and close contact with infected people are at high risk. The disease can be spread from person to person through small droplets in the nose or mouth when coughing or exhaling. These droplets stay on objects, and surfaces around the person. Then other people get infected with COVID-19 when touching these objects, or surfaces, and then touching their eyes, nose, or mouth. That is why it is important to maintain a-two-meter distance or more from someone who is sick. Given the importance of respiratory function over other systems of human body and the effects of the virus on this function, a systematic study could improve the evaluation and treatment protocols of people exposed to the virus. Such study can also be used by researchers as a scientific document including the findings of most studies conducted in the field.
Conflict of Interest Disclosures
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethical Statement
Not Applicable.
Acknowledgements
This research was financially supported by the Research Department at Shoushtar faculty of Medical Sciences. The researchers express their heartfelt gratitude to everyone involved in this study.
References
- Mudgal G. Structural Insights into Coronavirus Binding to Host Aminopeptidase N and Interaction Dynamics. Universidad Autónoma de Madrid; 2014.
- Fehr AR, Perlman S. Coronaviruses: an overview of their replication and pathogenesis. In: Maier H, Bickerton E, Britton P, eds. Coronaviruses. New York, NY: Humana Press; 2015. p. 1-23. 10.1007/978-1-4939-2438-7_1.
- Ghinai I, McPherson TD, Hunter JC, Kirking HL, Christiansen D, Joshi K. First known person-to-person transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the USA. Lancet 2020; 395(10230):1137-44. doi: 10.1016/s0140-6736(20)30607-3 [Crossref] [ Google Scholar]
- Farnoosh G, Alishiri G, Hosseini Zijoud SR, Dorostkar R, Jalali Farahani A. Understanding the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and Coronavirus Disease (COVID-19) Based on Available Evidence - A Narrative Review. J Mil Med 2020; 22(1):1-11. doi: 10.30491/jmm.22.1.1.[Persian] [Crossref] [ Google Scholar]
- Wu F, Zhao S, Yu B, Chen YM, Wang W, Song ZG. A new coronavirus associated with human respiratory disease in China. Nature 2020; 579(7798):265-9. doi: 10.1038/s41586-020-2008-3 [Crossref] [ Google Scholar]
- World Health Organization (WHO). Modes of Transmission of Virus Causing COVID-19: Implications for IPC Precaution Recommendations: Scientific Brief, 27 March 2020. WHO; 2020.
- World Organisation for Animal Health (OIE). Questions and answers about the 2019 Coronavirus Disease (COVID-19). Available from: https://wwwoieint/en/scientific-expertise/specific-information-and-recommendations/questions-and-answers-on-2019novel-coronavirus/.
- Han Q, Lin Q, Ni Z, You L. Uncertainties about the transmission routes of 2019 novel coronavirus. Influenza Other Respir Viruses 2020; 14(4):470-1. doi: 10.1111/irv.12735 [Crossref] [ Google Scholar]
- Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet 2020; 395(10223):470-3. doi: 10.1016/s0140-6736(20)30185-9 [Crossref] [ Google Scholar]
- Zhao S, Lin Q, Ran J, Musa SS, Yang G, Wang W. Preliminary estimation of the basic reproduction number of novel coronavirus (2019-nCoV) in China, from 2019 to 2020: a data-driven analysis in the early phase of the outbreak. Int J Infect Dis 2020; 92:214-7. doi: 10.1016/j.ijid.2020.01.050 [Crossref] [ Google Scholar]
- Institute NV (2020) Questions and answers about animals and coronavirus. Available from: https://wwwvetinstno/nyheter/koronavirus-pa-dyr-i-norge/sporsmal-og-svar-om-koronavirus-coronavirus.
- Chaudhuri S, Basu S, Saha A. Analyzing the dominant SARS-CoV-2 transmission routes toward an ab initio disease spread model. Phys Fluids (1994) 2020; 32(12):123306. doi: 10.1063/5.0034032 [Crossref] [ Google Scholar]
- Faridi S, Niazi S, Sadeghi K, Naddafi K, Yavarian J, Shamsipour M. A field indoor air measurement of SARS-CoV-2 in the patient rooms of the largest hospital in Iran. Sci Total Environ 2020; 725:138401. doi: 10.1016/j.scitotenv.2020.138401 [Crossref] [ Google Scholar]
- Ijaz MK, Brunner AH, Sattar SA, Nair RC, Johnson-Lussenburg CM. Survival characteristics of airborne human coronavirus 229E. J Gen Virol 1985; 66(Pt 12):2743-8. doi: 10.1099/0022-1317-66-12-2743 [Crossref] [ Google Scholar]
- Sun CB, Wang YY, Liu GH, Liu Z. Role of the eye in transmitting human coronavirus: what we know and what we do not know. Front Public Health 2020; 8:155. doi: 10.3389/fpubh.2020.00155 [Crossref] [ Google Scholar]
- Morawska L, Cao J. Airborne transmission of SARS-CoV-2: the world should face the reality. Environ Int 2020; 139:105730. doi: 10.1016/j.envint.2020.105730 [Crossref] [ Google Scholar]
- To KK, Tsang OT, Yip CC, Chan KH, Wu TC, Chan JM. Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis 2020; 71(15):841-3. doi: 10.1093/cid/ciaa149 [Crossref] [ Google Scholar]
- Tavakoli A, Vahdat K, Keshavarz M. Novel coronavirus disease 2019 (COVID-19): an emerging infectious disease in the 21st century. Iran South Med J 2020; 22(6):432-50. doi: 10.29252/ismj.22.6.432.[Persian] [Crossref] [ Google Scholar]
- Kutter JS, Spronken MI, Fraaij PL, Fouchier RA, Herfst S. Transmission routes of respiratory viruses among humans. Curr Opin Virol 2018; 28:142-51. doi: 10.1016/j.coviro.2018.01.001 [Crossref] [ Google Scholar]
- Zhang R, Li Y, Zhang AL, Wang Y, Molina MJ. Identifying airborne transmission as the dominant route for the spread of COVID-19. Proc Natl Acad Sci U S A 2020; 117(26):14857-63. doi: 10.1073/pnas.2009637117 [Crossref] [ Google Scholar]
- Wei J, Li Y. Airborne spread of infectious agents in the indoor environment. Am J Infect Control 2016; 44(9 Suppl):S102-8. doi: 10.1016/j.ajic.2016.06.003 [Crossref] [ Google Scholar]
- Duguid JP. The size and the duration of air-carriage of respiratory droplets and droplet-nuclei. J Hyg (Lond) 1946; 44(6):471-9. doi: 10.1017/s0022172400019288 [Crossref] [ Google Scholar]
- Jiang G, Wang C, Song L, Wang X, Zhou Y, Fei C. Aerosol transmission, an indispensable route of COVID-19 spread: case study of a department-store cluster. Front Environ Sci Eng 2021; 15(3):46. doi: 10.1007/s11783-021-1386-6 [Crossref] [ Google Scholar]
- da Silvia GM. An Analysis of the Transmission Modes of COVID-19 in Light of the Concepts of Indoor Air Quality. 2020. Available from: https://www.uc.pt/en/efs/Documentos/2020.04.06.
- Asadi S, Bouvier N, Wexler AS, Ristenpart WD. The coronavirus pandemic and aerosols: does COVID-19 transmit via expiratory particles?. Aerosol Sci Technol 2020; 54(6):635-8. doi: 10.1080/02786826.2020.1749229 [Crossref] [ Google Scholar]
- Yang S, Lee GW, Chen CM, Wu CC, Yu KP. The size and concentration of droplets generated by coughing in human subjects. J Aerosol Med 2007; 20(4):484-94. doi: 10.1089/jam.2007.0610 [Crossref] [ Google Scholar]
- Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020; 579(7798):270-3. doi: 10.1038/s41586-020-2012-7 [Crossref] [ Google Scholar]
- Lee BU. Minimum sizes of respiratory particles carrying SARS-CoV-2 and the possibility of aerosol generation. Int J Environ Res Public Health 2020; 17(19):6960. doi: 10.3390/ijerph17196960 [Crossref] [ Google Scholar]
- Bahl P, Doolan C, de Silva C, Chughtai AA, Bourouiba L, MacIntyre CR. Airborne or droplet precautions for health workers treating COVID-19? J Infect Dis. 2020. 10.1093/infdis/jiaa189.
- Galbadage T, Peterson BM, Gunasekera RS. Does COVID-19 spread through droplets alone?. Front Public Health 2020; 8:163. doi: 10.3389/fpubh.2020.00163 [Crossref] [ Google Scholar]
- Lindsley WG, Reynolds JS, Szalajda JV, Noti JD, Beezhold DH. A cough aerosol simulator for the study of disease transmission by human cough-generated aerosols. Aerosol Sci Technol 2013; 47(8):937-44. doi: 10.1080/02786826.2013.803019 [Crossref] [ Google Scholar]
- Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect 2020; 104(3):246-51. doi: 10.1016/j.jhin.2020.01.022 [Crossref] [ Google Scholar]
- Pandey D, Verma S, Verma P, Mahanty B, Dutta K, Daverey A. SARS-CoV-2 in wastewater: challenges for developing countries. Int J Hyg Environ Health 2021; 231:113634. doi: 10.1016/j.ijheh.2020.113634 [Crossref] [ Google Scholar]
- Langone M, Petta L, Cellamare CM, Ferraris M, Guzzinati R, Mattioli D. SARS-CoV-2 in water services: presence and impacts. Environ Pollut 2021; 268(Pt A):115806. doi: 10.1016/j.envpol.2020.115806 [Crossref] [ Google Scholar]
- Twaddell OE. COVID-19 and Drinking Water: An Update Amid Further Scrutiny. Goldberg Segalla LLP; 2020. Available from: https://www.lexology.com/library/detail.aspx?g=1cdde46d-efb7-400c-af7e-85e629e62b02.
- Arslan M, Xu B, Gamal El-Din M. Transmission of SARS-CoV-2 via fecal-oral and aerosols-borne routes: environmental dynamics and implications for wastewater management in underprivileged societies. Sci Total Environ 2020; 743:140709. doi: 10.1016/j.scitotenv.2020.140709 [Crossref] [ Google Scholar]