Avicenna J Environ Health Eng. 9(2):100-108.
doi: 10.34172/ajehe.2022.5296
Review
A Narrative Review of the Survival of the Coronavirus Family in Feces, Urine, and Wastewater
Seyedeh Fatemeh Mousavi 1  , Fathollah Gholami-Borujeni 2, *
, Fathollah Gholami-Borujeni 2, * 
Author information:
1MSc of Environmental Health Engineering, Students Research Committee, Mazandaran University of Medical Sciences, Sari, Iran
2Department of Environmental Health Engineering, Faculty of Health, Mazandaran University of Medical Sciences, Sari, Iran
Abstract
Wastewater is one of the most important ways of transmitting viral and bacterial pathogens that can cause nosocomial and clinical infections in humans. Although previous studies show that there is no current evidence that active coronaviruses are present in surface or ground waters or are transmitted through contaminated drinking water, there is an urgent need for more effective preventive measures to limit the spread of infection, which depends on understanding their routes of transmission and persistence in different environments. Here is a narrative review of the survival of the coronavirus family in feces, urine, and wastewater. Articles related to the presence of SARS-CoV-1 and SARS-CoV-2 in feces, urine, and wastewater and their survival time were searched in the literature. Articles published in the last decade (2000–2021) were selected based on the PRISMA method. The literature review showed that due to the high concentration of RNA virus in blood and urine samples with positive oral and anal swabs, no positive case has been reported using respiratory tests. The main findings of this review show that the maximum survival time of the SARS-CoV-2 in feces and urine was 33 and 31 days, respectively. Moreover, environmental conditions (temperature and pH) are the most important factors in the survival of SRRS-CoV in feces, urine, and wastewater. This study provides researchers with basic and useful information for future research orientations in relation to wastewater treatment plant systems to eliminate and manage emerging viral contaminants.
Keywords: SARS COV-2, Survival, Wastewater, Feces, Urine,
Copyright and License Information
© 2022 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Please cite this article as follows: Mousavi SF, Gholami-Borujeni F. A narrative review of the survival of the coronavirus family in feces, urine, and wastewater. Avicenna J Environ Health Eng. 2022; 9(2):100-108. doi:10.34172/ajehe.2022.5296
1. Introduction
Pandemics are common phenomena in human life history that occur on average once every 30 years and lead to human morbidity and mortality worldwide (1). Coronavirus disease 2019 (COVID-19), which started in late 2019, has now become a global epidemic and has spread to all countries of the world (2). In 2002, acute respiratory syndrome and the recently emerging Middle East respiratory syndrome (MERS), with many communities involved, can be described as threats to human health. About 17 years ago, a new acute respiratory disease occurred in China. The first case of the disease was identified in Guangdong province, China. The patient was a 45-year-old man with respiratory symptoms and fever (3). It spread to most provinces and countries all over the world (4). Severe acute respiratory syndrome (SARS) spread from person to person in family members or health care providers (5). Accordingly, the illness affected many people in the United States, Europe, and Asia (6). The diseases can be difficult to detect if people are more likely to travel and not to observe social distance. Therefore, the availability of early diagnostic tests reduces the spread of the disease. Reverse transcription-polymerase chain reaction (RT-PCR) test is required for early detection (7). World Health Organization (WHO) and the Centers for Disease Control (CDC) provide guidelines for communities, indicating that handwashing and the use of masks can be effective strategies to prevent transmission of the virus (8). However, numerous studies indicate that Severe acute respiratory syndrome coronavirus (SARS-CoV) can survive in food, water, and wastewater for a long time (9,10). The contamination of water supplies through wastewater discharge has been historically recognized as a risk factor for human health. The water consumption of communities can cause the spread of pathogens, creating the conditions for outbreaks or sporadic cases of infectious diseases. Human pathogens such as bacteria, worms, protozoa, and viruses are often detected in water environments and are considered to be responsible for a considerable proportion of waterborne diseases. The presence of contaminants in wastewater is the reason for ongoing monitoring which can increase the preparedness of utilities to respond to public health problems (11). Wastewater containing the Ebola virus is discharged directly into the wastewater collection system without any treatment (11). Gastrointestinal symptoms such as diarrhea, nausea, and vomiting have been reported among patients during the COVID-19 outbreak (12,13). Literature review showed that SARS-CoV -2 is transmitted through aerosols. Transmission through water and wastewater resource has not been reported yet. Although the virus may survive in drinking water and wastewater, there is no evidence that SARS-CoV-2 can be transmitted through contaminated drinking water (13). Generally, there are more viruses in the winter than in the summer in the wastewater treatment plants, which can be mostly related to gastrointestinal diseases or poliomyelitis caused by enterovirus, hepatitis (A and E), norovirus, and other Caliciviruses (14). Some research findings indicated that SARS-CoV-1 and SARS-CoV-2 can survive for 4-72 hours and under different environmental conditions, this survival time varies from 4 hours to 31 days (15). According to Wang et al, SARS-CoV can survive for 2-14 days at 20-24°C in wastewater (16). Based on the results of the study conducted by Duan et al, SARS-CoV is stable in the environment and can survive for at least 96 hours in feces and on surfaces at room temperature. It remains in the urine for up to 72 hours at a low infectious dose. However, at 20-37°C, it remains for at least 2 hours. Radiation was reported to inactivate the virus in 60 minutes (3). Knowing the survival time of viruses in different environments can be of great importance for making decisions about control and preventive measures for the spread of contamination in human populations. The purpose of this study was to review the survival of the coronavirus family in feces, urine, and wastewater.
2. Materials and Methods
2.1. Search Strategies
PubMed, Scopus, and Web of Science databases were searched independently for articles published in English up to November 6, 2021. The keywords used in the search were “Coronavirus” and “SARS” and “Ebola” and “MERS” and “Survival” and “Water and Wastewater” and “Stool” and “Feces” and “Fecal’’. The main data of the articles were collected and categorized. Three data extraction tables were developed to collect data on the important finding, method of detection, and survival period of the virus in wastewater, feces, and urine. The keywords consisting “coronavirus” OR “SARS CoV” OR “Urine” OR “feces” OR “wastewater” OR “detection” AND “stool” OR “water” were used.
2.2. Paper Selection Criteria
The criterion for the selection of articles was access to original English full-text articles reporting the detection and survival of coronavirus in feces, urine, and wastewater. In addition, letters to editors, review articles, chapters, books, conferences, and duplicate papers were excluded. Country, types of environment (faces, urine, and wastewater), detection method, minimum and maximum survival times, and type of virus were considered in this study. Additionally, studies published in non-English languages were excluded from the study. Articles published in the last decade (2000–2021) were selected based on the PRISMA method. Summary of standard four-steps protocol for literature review is shown at Fig. 1.
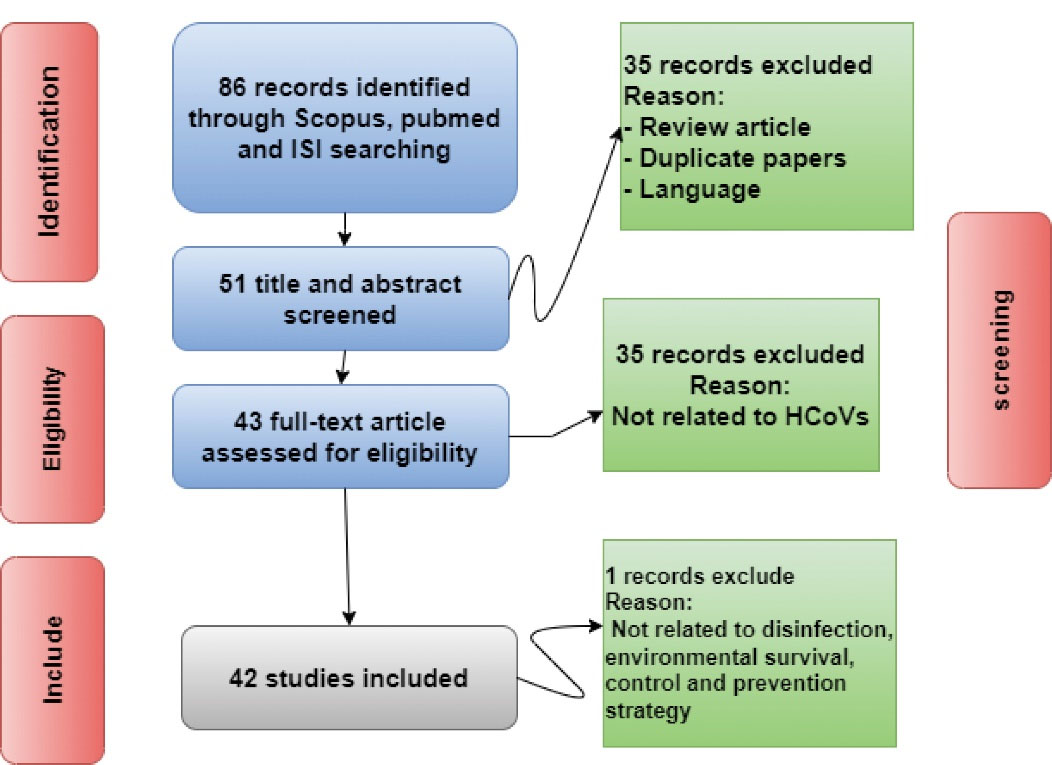
Fig. 1.
Summary of a Standard Four-step Protocol for Literature Review
.
Summary of a Standard Four-step Protocol for Literature Review
3. Results and Discussion
All the data analyzed were related to the coronavirus family. According to the findings of the present study, the half-life of these viruses varies according to their type. The coronavirus is transmitted from a person who has diarrhea and the virus is present in his/her diarrhea for 22 days and remains in the pasteurized sludge for 9 days (17). For SARS-CoV, it is 73 hours to 14 days, depending on the temperature and the laboratory environment. The survival of Ebola virus varies from 8 to 19 days in the sewers of various places and it remains in the blood serum for up to 46 days. MERS-CoV has been reported to be active in the urine for up to 13 days. It is noteworthy that with the increase of the temperature, the viability and activity of these viruses were decrease. SARS-CoV 2 survived in feces for 1-33 days and in urine for 3-22 days (Table 1) (2). In some studies, urine tests were negative despite the presence of the virus in the feces. In general, the survival of viruses varies depending on the temperature, the organic matter, and presence of antagonistic bacteria. Having complete and comprehensive information about virus transmission is vital for enhancing health in communities. The concentrations of viruses in bioaerosols of wastewater treatment plants were measured for their effect on the health of workers and residents over a 20-month period. The viral loads were significantly higher than the threshold values recommended by the U.S. Environmental Protection Agency (US EPA) (18). Gastrointestinal symptoms such as diarrhea, nausea, and vomiting have been reported among patients during the outbreak of SARS-CoV-2. Importantly, patients with a positive stool test had no gastrointestinal symptoms and this was not associated with the severity of the lung infection. The temperature and duration of wastewater reaching the municipal wastewater treatment plant are effective in detecting the virus (Table 2). According to experiments, the survival time of the virus in water at 23°C was 2-4 days, considering the effects of temperature, organic matter level, and presence of antagonistic bacteria (19). Laboratory scale studies indicate that the survival time of coronavirus can range from days to weeks. It should be kept in a clean, covered container in order to preserve treated water. In addition, filtration and disinfection can help to inactivate the virus in pandemics (20). Individuals may be infected by inhalation of virus-infected aerosols, but the risk of transmission is lower in direct contact with feces (21). Review of the literature shows that there is no strong evidence for the transmission of SARS-CoV-2 viruses through water and wastewater right now (22). So far there has been no general conclusion that contaminated wastewater can transmit the virus. In addition, there was no conclusion that wastewater causes SARS. But it is better to consider wastewater treatment lagoons for 20 days retention time rather than other critical parameters such as temperature and pH. Using disinfectants is another strategy for inactivating coronaviruses. The use of personal protective equipment is recommended to protect healthcare workers and those working in wastewater treatment plants (23). Sodium hypochlorite is used as a disinfectant in health guidelines. Based on the laboratory data, the survival of SARS-CoV at room temperature (25°C) in feces and urine was reported to be 2 and 14 days, respectively (16). As shown, the maximum survival time of SARS-CoV-2 in feces was 33 days (24). In most cases, urine tests were negative, but in the study of Zheng et al, a duration of 31 days was reported (25) (Table 3). Personnel with direct contact with infected patients should use personal protective equipment such as gowns, masks, shields, and disposable gloves. Additionally, infected persons should be prevented from entering sterile areas, diagnostic rooms, and medical equipment storage rooms (26).
Table 1.
Studies on the Survival Time of Coronavirus Family Published before COVID-19 Pandemic
|
Coronavirus Type
|
Important Findings
|
Source of Sampling
|
Reference
|
| SARS |
SARS-CoV can survive for 2-14 days in 20-24°C, respectively. The virus was inactivated after 8 days. They found that SARS-CoV cannot be alive after disinfection but it can still be detected. |
Wastewater |
(16) |
| SARS |
Viruses can be active in wastewater.
They may be inactivated by treatment or disinfection. |
Wastewater |
(27) |
| SARS |
Generally, more viruses can be detected in the winter than in the summer in the wastewater. They have realized that pathogens may exist in wastewater.
Maximum disinfection should be carried out during the swimming seasons as effluent enters the sea. |
Wastewater |
(28) |
| SARS |
They found that although SARS spreads through respiratory droplets, approximately in 50% of patients infected with SARS, the virus was detected in the feces for 10 weeks. |
Feces |
(29) |
| SARS |
SARS-CoV is stable in the environment and can survive at least for 96 hours in feces and on surfaces at room temperature.
It remains in the urine for up to 72 hours at a low infectious dose. However, at 20-37°C, it remains for at least 2 hours. Radiation inactivated the virus in 60 minutes. |
Feces, urine |
(3) |
| SARS |
They reported that SARS had a low rate of viral shedding in the early days. In fluids secreted from the upper respiratory system and feces, the virus was detected on the 14th day. |
Upper respiratory tract, faces |
(30) |
| SARS |
They concluded that due to the ability of the SARS-CoV to replicate in the intestine, it was found on the 73th day. |
Feces |
(31) |
| MERS-Cov |
In the sample taken from a 73-year-old, the maximum amount of MERS-CoV in the urine was detected on day 13. After the kidney failure on the 14th day, the test was negative. |
Urine |
(32) |
| Ebola |
Ebola virus was inactivated at a high temperature within 7 days, and inactivation occurred at 30°C faster than 22°C. |
Wastewater |
(17) |
| SARS |
SARS-CoV can survive at room temperature in alkaline feces for up to 4 days. All disinfectants reduced the virus load by > 3 log within 5 minutes. |
Feces |
(33) |
| Transmissible gastroenteritis |
Coronavirus stays in water and wastewater for 22 days, it sometimes causes gastroenteritis.
It remains in water at 25°C for 22 days and remains in pasteurized wastewater sludge for 9 days. |
Water, waste water |
(34) |
| SARS |
In vitro experiments indicated that SARS survived in the home and hospital wastewater environments for 2 days at 4-25°C and in feces for 14-3 days at 4-25°C, respectively. At the same temperatures (4-25°C), it remained in the urine for 17 days. |
Feces, urine, water. |
(16) |
| Ebola |
The survival of Ebola virus was reported to be over 18 days in hospital wastewater and human feces. Based on the results, 5 log10 reduction occurred on day 8. The virus was inactivated in shorter time at 37°C than at 22°C. |
Wastewater, feces |
(35) |
| Ebola |
The results showed that the Ebola virus titer decreased 90% on first days, which could be due to the inactivation of the viral particles.
Ebola virus was less stable than intestinal viruses. |
Wastewater |
(36) |
| Coronaviruses |
Survival of coronavirus depends on the water temperature, organic matter, and the antagonistic bacteria.
The virus become inactive within 10 or more than 1000 days.
They found that the virus survived in wastewater for about 2-4 days. |
Water, Wastewater |
(19) |
| Ebola |
The virus was inactivated after 20 seconds by adding 5-10 mg/L of sodium hypochlorite (PH increased to 11.2). |
Wastewater |
(37) |
| Ebola |
Ebola virus survived in feces and urine for 19 and 30 days, respectively. |
Feces, urine |
(38) |
| SARS |
SARS-CoV was detected in the feces in 6 to 90 hours. |
Feces, urine |
(39) |
| SARS |
SARS-CoV was detected at room temperature in the feces and urine at least 2 and less than 24 hours, respectively. |
Feces, urine |
(40) |
| Ebola virus |
Ebola virus survived in different fluids for a longer period of time, as it persists in the serum for 56 days. |
Serum |
(41) |
Table 2.
Studies on the Survival Time of SARS-CoV-2 Published During COVID-19 Pandemic
|
Country
|
City/Region
|
Source
|
Detection Method
|
Type of Disinfection
|
Population
|
Year
|
Important Finding
|
Reference
|
| Australia |
Monte-Carlo |
Wastewater |
RT-qPCR |
NR |
600 000 |
2020 |
SARS-CoV-2 was detected in wastewater over 6 days in this study. Grab sampling techniques was used. Two methods including direct RNA extraction and ultrafiltration were used. The sensitivity analysis showed 10 log/g SARS-CoV-2 RNA copies in feces and wastewater. |
(42) |
| China |
Wuhan |
Diarrhea, nausea, and vomiting |
NR |
NR |
NR |
2020 |
Gastrointestinal symptoms such as diarrhea, nausea, and vomiting have been reported among patients during the COVID-19 outbreak. The virus can be transmitted through infected hands. In this study, the use of probiotics to improve gastrointestinal symptoms and protect the respiratory system is recommended. |
(12) |
| The United States |
Snohomish County, Washington |
Serum, urine and Feces samples |
RT-qPCR |
NR |
Case study |
2020 |
Serum and fecal samples were negative in both collection dates and positive after 7 days of illness, respectively. |
(43) |
| China |
Shanghai, Hainan, and Hefei |
Urine and feces samples |
Nucleic acid detection |
NR |
10 Cases
(children) |
2020 |
The presented study showed that in 10 identified infected children, 6 patients have been identified as positive in a fecal sample for 3 to 13 days after illness onset. Additionally, 2 patients had negative tests 10 days after the onset of the disease.
Urine and serum samples were negative for 2 to 3 days after the onset of the disease. |
(26) |
| China |
NR |
Feces |
RT-qPCR |
NR |
Case study |
2020 |
Despite the negative respiratory test, the child's fecal test was positive 26 days after the onset of the disease. |
(44) |
| China |
NR |
Blood and urine |
RT-qPCR |
NR |
9 Cases
(hospitalized patients) |
2020 |
Due to the high concentration of RNA virus in blood and urine samples, no positive case has been reported using respiratory tests. |
(45) |
| China |
Wuhan |
Blood and serum |
qRT-PCR |
NR |
16 Cases (patients) |
2020 |
Of the 15 patients with SARS-CoV-2 in this study, 8 oral tests, 4 anal tests, 6 blood tests, and 3 serum positive tests were reported on the first day. However, after 5 days, only 4 people had a positive oral test. A very interesting point in this study was that none of the patients with viremia blood had a positive oral and anal swabs. |
(46) |
| China |
Jinhua Municipal Central |
Feces |
Nucleic acid detection |
NR |
14 Cases (patients) |
2020 |
Importantly, patients with a positive fecal test had no gastrointestinal symptoms and this was not associated with the severity of lung infection. |
(26) |
| The United States |
Tempe, Arizona, |
Feces |
RT-qPCR |
NR |
185 038 |
2020 |
The temperature and duration of wastewater reaching the municipal wastewater treatment plant are effective in detecting the virus. The half-life of SARS-CoV-2 at 20°C in most wastewater systems worldwide is reported to be approximately 4.8 and 7.2 hours, respectively. |
(47) |
| The Netherlands |
Amsterdam Airport Schiphol, Haarlemmermeer |
Human wastewater |
RT-PCR |
NR |
NR |
2020 |
24-hour 10 L samples taken from human wastewater were tested positive for the presence of viral RNA. |
(48) |
| Australia |
Brisbane, Queensland |
Untreated wastewater |
RT-qPCR |
NR |
198 000, 505 000, and 231 000, for Plant A, B, and C, respectively |
2021 |
From three wastewater treatment plants, 63 composite samples were taken, and 21 cases of SARS-CoV-2 were reported positive. The number of copies of SARS-CoV-2 RNA in wastewater was not related to the number of daily cases, which can be attributed to the characteristics of the basin, collection system, and duration time. |
(10) |
| Italy |
Milan and Rome |
Influent wastewater |
RT-PCR |
NR |
105 000 |
2020 |
Six of the total 24-hour composite samples (n = 12) were identified as positive effluents.
It is recommended that the WHO protocol be used for wastewater treatment during the virus outbreak after appropriate modifications. |
(49) |
| Italy |
Milano and Monza e Brianza |
Raw and treated wastewater |
RT-PCR |
|
480 000 population and 4.500 industrial facilities |
2020 |
The presence of SARS-CoV-2 RNA was detected, indicating a residue at the effluent outlet confirming that secondary treatment may also have residual RNA in the effluent. The river water receiving SARS-CoV-2 was zero. Despite viral RNA in urine and feces, it cannot be infected. In addition, testing for infectivity has shown that virus pathogenicity in wastewater can be zero, whether in raw or treated samples and surface water. |
(50) |
| China |
Zhejiang |
Wastewater |
qRT-PCR |
|
33 Laboratory-confirmed patients |
2020 |
SARS-CoV-2 was positive in the samples of the patients, while the respiratory and fecal samples of the patient were positive in a room with mechanical ventilation and negative without mechanical ventilation. The risk of infection from wastewater and rivers is negligible. |
(46) |
| Singapore |
Singapore |
Feces |
RT-PCR |
NR |
3 Cases isolation rooms |
2020 |
The patient with respiratory problems, who had not reached the pneumonia stage, had no gastrointestinal symptoms such as diarrhea but had a positive SARS-CoV-2 fecal test. |
(51) |
| France |
Parisian area |
Feces, raw wastewater |
RT-qPCR |
NR |
100 000 Cases inhabitants |
2020 |
This study showed that the onset of SARS-CoV-2 occurred before the onset of clinical symptoms in affected individuals. In addition, the results showed that it stays in the wastewater for a long time |
(52) |
| The United States |
Massachusetts |
Raw wastewater of urban origin |
RT-qPCR |
NR |
7000 Individuals |
2020 |
The number of positive cases of SARS-CoV-2 in wastewater is higher than the number of infected cases, which may cause transmission of the disease to healthy people.
Viral titers in feces have been reported to be about 3000 times higher compared to raw wastewater samples. |
(53) |
| Spain |
Murcia |
Influent, secondary and tertiary effluent |
RT-qPCR |
NR |
100 000 Inhabitants |
2020 |
RNA removal efficiency of SARS-CoV virus from input to secondary sedimentation and finally advanced purification has varied between 20% and 100%. |
(54) |
| Turkey |
Ambarli, Pasakoy and Kadikoy |
Raw wastewater |
RT-qPCR |
NR |
600 000
People |
2020 |
SARS-CoV-2 was positive in 5 out of 7 samples taken from raw wastewater. However, all samples taken from manholes were positive. The virus titers of raw wastewater from the manhole were higher than those of the inlet of wastewater treatment plants. These amounts decreased overtime in the wastewater treatment plant. |
(55) |
| Bangladesh |
Noakhali |
Wastewater |
RT-PCR |
NR |
NR |
2021 |
The results showed that temporal changes in the load of SARS-CoV-2 RNA in wastewater are reduced.
In this study, the time interval was not measurable due to different discharge sites containing virus RNA. However, changes in the environment such as temperature fluctuations and humidity are effective in virus residues. |
(56) |
| France |
Parisian area |
Raw wastewater |
RT-qPCR |
NR |
More than 100 000
inhabitants |
2020 |
With the increase in the number of patients, the amount of SARS-CoV-2 genome has increased dramatically and the presence of SARS-CoV-2 in all municipal wastewater samples was confirmed. There were no changes in the concentration of viruses in the raw wastewater during the assessed period because of no significant rain fall. |
(57) |
| The Netherlands |
Dutch |
Wastewater |
qRT-PCR |
NR |
6 Cities |
2020 |
Wastewater samples were positive for each assay. |
(58) |
| Italy |
Milano |
Raw and treated wastewater |
RT-PCR |
UV |
2 million
persons |
2020 |
SARS-CoV-2 RNA was detected in the incoming stream but not in the effluent. With epidemiological changes, the amount of virus genome detected decreased after 8 days. |
(50) |
| The United States |
Northern Indiana |
Municipal wastewater |
NR |
NR |
NR |
2020 |
SARS-CoV-2 remained at room temperature in wastewater and tap water for 1.5 and 1.7 days, respectively. In this study, the virus genome remained in the high-titrated wastewater for 7 days.
SARS-CoV-2 survives for 15 and 2 minutes at 50 and 70°C in wastewater, respectively. SARS-CoV-2 has been reported to survive in untreated wastewater for 20.4 and 12.6 days at 15 and 25°C, respectively. |
(59) |
| Australia |
Brisbane |
Wastewater |
RT-qPCR |
NR |
325 000 People |
2020 |
The temperature had the greatest effect on the first-order decay rate of SARS-CoV-2 RNA.
SARS-CoV-2 RNA T90 (time required for 1 log10 reduction) ranged from 8.04 to 27.8 days in untreated wastewater, 5.71 to 43.2 days in autoclaved wastewater, and 9.40 to 58.6 days in tap water. |
(59) |
| Italy |
Cremona |
Feces and urine |
RT-PCR |
NR |
411 Patients |
2020 |
SARS-CoV-2 RNA can be detected in feces and urine. In watery diarrhea, it survives for about 3 hours to 5 days.
The possibility of transmitting SARS-CoV-2 through feces is very low. |
(60) |
| Italy |
Rome |
Feces |
RT-PCR |
NR |
15 Patients |
2020 |
Fifteen days after the first positive respiratory test, 6 fecal samples from 15 infected patients were positive. Fecal samples were positive 25 days after the onset of the disease. |
(61) |
| China |
Guangzhou |
Feces |
RT-PCR |
NR |
745 ‘Highly suspected’ children |
2020 |
Children in this study did not need respiratory support or intensive care. Eight children had positive rectal swabs after a negative respiratory test, which increased the risk of fecal-oral transmission. Some children had a positive rectal test for up to 13 days after recovery. The probability of a positive fecal test increases. |
(51) |
| China |
Tianjin |
Feces |
RT-PCR |
NR |
3 Infected children |
2020 |
Ten days after recovery, all patients and their families were reported to have positive fecal test results.
Most children do not have acute symptoms of SARS-CoV-2. |
(21) |
| China |
Shandong University, Jinan |
Feces and urine |
RT-PCR |
NR |
10 Infected children |
2020 |
The approximate time of negative RT-PCR test from the beginning of diagnosis for respiratory and fecal tests was 9 days and 34.43 days, respectively.
After 2 weeks of discharge from the hospital, there were 7 positive SARS-CoV-2 fecal tests, while urine and respiratory samples were negative. |
(62) |
Table 3.
Studies on the Survival Time of SARS-CoV-2 in Feces and Urine Published During Pandemic
|
Author
|
Type of Sample
|
Survival Time
|
Country
|
Reference
|
| Wang et al |
Feces |
23.55-26.45 days |
China |
(63) |
| Chan et al |
Feces |
1–2 Days (at room temperature) |
China |
(64) |
| Liu et al |
Feces and urine |
Adult: 2 hours, child: 2 days in feces
Adult: 3 days, child: 4 days in a urine sample |
China |
(14) |
| Zheng et al |
Feces and Urine |
22 days, interquartile range 17-31 days |
China |
(25) |
| Chen et al |
Feces |
6-10 Days |
China |
(65) |
| Zhang et al |
Feces |
10 Days |
China |
(66) |
| Xing et al |
Feces |
20 Days |
China |
(67) |
| Wu et al |
Feces |
33 Days |
China |
(24) |
| Kim et al |
Feces and Urine |
5-12 Days |
Korea |
(68) |
| Ling et al |
Feces |
11-20 Days |
China |
(69) |
| Lo et al |
Feces |
19.3 Days |
China |
(70) |
| Zhang et al |
Feces |
22.0 Days |
China |
(71) |
| Xiao et al |
Feces |
1 to 12 Days |
China |
(72) |
4. Conclusion
Coronavirus can survive in filtered drinking water at 23°C for approximately 2-14 days. It can survive for up to 9 days in pasteurized sludge. Disinfectants can reduce SARS-CoV load by > 3 log within 5 minutes. The present study showed that SARS-CoV, MERS-CoV and Ebola virus can survive for 2-14 days in filtered drinking water at 23°. Accordingly, coronavirus can be inactivated at 23°C and 25°C within 2-12 days, respectively. Common disinfectants such as 70% ethanol and sodium hypochlorite can be used for inactivation within 1 minute. The transmission risk of the disease through the feces is low, but it can cause diarrhea and intestinal infection by swallowing. The maximum survival time of SARS-CoV-2 in feces and urine was reported to be 33 and 31 days, respectively. The findings of this review show that various factors can affect the survival time of the virus in different environments. Therefore, the survival time of the SARS-CoV in feces, urine, and wastewater has been reported to be very variable, and this time has been reported to range from a few hours to 31 days. Environmental conditions (temperature and pH) are the most important factors in the survival of SARS-CoV in feces, urine, and wastewater. Further studies are needed to investigate the potential presence and fate of coronavirus and other enveloped viruses in feces, urine, and wastewater, as well as drinking water
Acknowledgements
This survey was supported by the Deputy of Research and Technology of Mazandaran University of Medical Sciences of Iran (IR.MAZUMS.REC.1399.038).
Authors’ Contribution
Conceptualization: Fathollah Gholami-Borujeni, Seyedeh Fatemeh Mousavi.
Methodology: Fathollah Gholami-Borujeni, Seyedeh Fatemeh Mousavi.
Validation: Fatemeh Mousavi.
Formal Analysis: Seyedeh Fatemeh Mousavi.
Investigation: Seyedeh Fatemeh Mousavi.
Resources: Fathollah Gholami-Borujeni.
Data Curation: Seyedeh Fatemeh Mousavi.
Writing—Original Draft Preparation: Seyedeh Fatemeh Mousavi.
Writing—Review and Editing: Fathollah Gholami-Borujeni.
Visualization: Fathollah Gholami-Borujeni.
Supervision: Fathollah Gholami-Borujeni.
Project Administration: Fathollah Gholami-Borujeni.
Funding Acquisition: Fathollah Gholami-Borujeni.
Competing Interests
The authors declare that they have no conflict of interest.
Ethical Approval
The conducted research is not related to either human or animal use.
References
- Spinelli A, Pellino G. COVID-19 pandemic: perspectives on an unfolding crisis. Br J Surg 2020; 107(7):785-7. doi: 10.1002/bjs.11627 [Crossref] [ Google Scholar]
- World Health Organization (WHO). Coronavirus Disease 2019 (COVID-19) Situation Report 46. Geneva: WHO; 2020.
- Das Adhikari U, Eng G, Farcasanu M. Fecal Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-Cov-2) RNA Is Associated With Decreased Coronavirus Disease 2019 (COVID-19) Survival. Clin Infect Dis 2022; 74(6):1081-1084. doi: 10.1093/cid/ciab623 [Crossref] [ Google Scholar]
- Adhikari U, Chabrelie A, Weir M, Boehnke K, McKenzie E, Ikner L. A case study evaluating the risk of infection from Middle Eastern respiratory syndrome coronavirus (MERS-CoV) in a hospital setting through bioaerosols. Risk Anal 2019; 39(12):2608-24. doi: 10.1111/risa.13389 [Crossref] [ Google Scholar]
- Leung CW, Chiu WK. Clinical picture, diagnosis, treatment and outcome of severe acute respiratory syndrome (SARS) in children. Paediatr Respir Rev 2004; 5(4):275-88. doi: 10.1016/j.prrv.2004.07.010 [Crossref] [ Google Scholar]
- Peiris JS, Lai ST, Poon LL, Guan Y, Yam LY, Lim W. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet 2003; 361(9366):1319-25. doi: 10.1016/s0140-6736(03)13077-2 [Crossref] [ Google Scholar]
- Falsey AR, Walsh EE. Novel coronavirus and severe acute respiratory syndrome. Lancet 2003; 361(9366):1312-3. doi: 10.1016/s0140-6736(03)13084-x [Crossref] [ Google Scholar]
- Olsen SJ, Chang HL, Cheung TY, Tang AF, Fisk TL, Ooi SP. Transmission of the severe acute respiratory syndrome on aircraft. N Engl J Med 2003; 349(25):2416-22. doi: 10.1056/NEJMoa031349 [Crossref] [ Google Scholar]
- Eslami H, Jalili M. The role of environmental factors to transmission of SARS-CoV-2 (COVID-19). AMB Express 2020; 10(1):92. doi: 10.1186/s13568-020-01028-0 [Crossref] [ Google Scholar]
- Ahmed W, Tscharke B, Bertsch PM, Bibby K, Bivins A, Choi P. SARS-CoV-2 RNA monitoring in wastewater as a potential early warning system for COVID-19 transmission in the community: a temporal case study. Sci Total Environ 2021; 761:144216. doi: 10.1016/j.scitotenv.2020.144216 [Crossref] [ Google Scholar]
- Sinclair RG, Choi CY, Riley MR, Gerba CP. Pathogen surveillance through monitoring of sewer systems. Adv Appl Microbiol 2008; 65:249-69. doi: 10.1016/s0065-2164(08)00609-6 [Crossref] [ Google Scholar]
- Gao QY, Chen YX, Fang JY. 2019 Novel coronavirus infection and gastrointestinal tract. J Dig Dis 2020; 21(3):125-6. doi: 10.1111/1751-2980.12851 [Crossref] [ Google Scholar]
- Jaafarzadeh N, Jorfi S, Ghaedrahmat Z, Almasi H, Zahedi A. Transmission routes of COVID-19 through air, water and wastewater: a systematic review. Avicenna J Environ Health Eng 2020; 7(2):109-17. doi: 10.34172/ajehe.2020.16 [Crossref] [ Google Scholar]
- Liu Y, Li T, Deng Y, Liu S, Zhang D, Li H. Stability of SARS-CoV-2 on environmental surfaces and in human excreta. J Hosp Infect 2021; 107:105-7. doi: 10.1016/j.jhin.2020.10.021 [Crossref] [ Google Scholar]
- Noorimotlagh Z, Mirzaee SA, Jaafarzadeh N, Maleki M, Kalvandi G, Karami C. A systematic review of emerging human coronavirus (SARS-CoV-2) outbreak: focus on disinfection methods, environmental survival, and control and prevention strategies. Environ Sci Pollut Res Int 2021; 28(1):1-15. doi: 10.1007/s11356-020-11060-z [Crossref] [ Google Scholar]
- Wang XW, Li J, Guo T, Zhen B, Kong Q, Yi B. Concentration and detection of SARS coronavirus in sewage from Xiao Tang Shan Hospital and the 309th Hospital of the Chinese People’s Liberation Army. Water Sci Technol 2005; 52(8):213-21. [ Google Scholar]
- Casanova LM, Weaver SR. Inactivation of an enveloped surrogate virus in human sewage. Environm Sci Technol Lett 2015; 2(3):76-8. doi: 10.1021/acs.estlett.5b00029 [Crossref] [ Google Scholar]
- Pasalari H, Ataei-Pirkooh A, Aminikhah M, Jonidi Jafari A, Farzadkia M. Assessment of airborne enteric viruses emitted from wastewater treatment plant: atmospheric dispersion model, quantitative microbial risk assessment, disease burden. Environ Pollut 2019; 253:464-73. doi: 10.1016/j.envpol.2019.07.010 [Crossref] [ Google Scholar]
- Gundy PM, Gerba CP, Pepper IL. Survival of coronaviruses in water and wastewater. Food Environ Virol 2008; 1(1):10. doi: 10.1007/s12560-008-9001-6 [Crossref] [ Google Scholar]
- Yeo C, Kaushal S, Yeo D. Enteric involvement of coronaviruses: is faecal-oral transmission of SARS-CoV-2 possible?. Lancet Gastroenterol Hepatol 2020; 5(4):335-7. doi: 10.1016/s2468-1253(20)30048-0 [Crossref] [ Google Scholar]
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395(10223):497-506. doi: 10.1016/s0140-6736(20)30183-5 [Crossref] [ Google Scholar]
- Gorchev HG, Ozolins G. WHO guidelines for drinking-water quality. WHO Chron 1984; 38(3):104-8. [ Google Scholar]
- World Health Organization (WHO). Water, Sanitation, Hygiene and Waste Management for COVID-19: Technical Brief, 3 March 2020. WHO; 2020.
- Wu Y, Guo C, Tang L, Hong Z, Zhou J, Dong X. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol Hepatol 2020; 5(5):434-5. doi: 10.1016/s2468-1253(20)30083-2 [Crossref] [ Google Scholar]
- Zheng S, Fan J, Yu F, Feng B, Lou B, Zou Q. Viral load dynamics and disease severity in patients infected with SARS-CoV-2 in Zhejiang province, China, January-March 2020: retrospective cohort study. BMJ 2020; 369:m1443. doi: 10.1136/bmj.m1443 [Crossref] [ Google Scholar]
- Jiehao C, Jin X, Daojiong L, Zhi Y, Lei X, Zhenghai Q. A case series of children with 2019 novel coronavirus infection: clinical and epidemiological features. Clin Infect Dis 2020; 71(6):1547-51. doi: 10.1093/cid/ciaa198 [Crossref] [ Google Scholar]
- Cliver DO. Control of viral contamination of food and environment. Food Environ Virol 2009; 1(1):3-9. doi: 10.1007/s12560-008-9005-2 [Crossref] [ Google Scholar]
- Wong MV, Hashsham SA, Gulari E, Rouillard JM, Aw TG, Rose JB. Detection and characterization of human pathogenic viruses circulating in community wastewater using multi target microarrays and polymerase chain reaction. J Water Health 2013; 11(4):659-70. doi: 10.2166/wh.2013.322 [Crossref] [ Google Scholar]
- Leung WK, To KF, Chan PK, Chan HL, Wu AK, Lee N. Enteric involvement of severe acute respiratory syndrome-associated coronavirus infection. Gastroenterology 2003; 125(4):1011-7. doi: 10.1016/s0016-5085(03)01215-0 [Crossref] [ Google Scholar]
- Cheng PK, Wong DA, Tong LK, Ip SM, Lo AC, Lau CS. Viral shedding patterns of coronavirus in patients with probable severe acute respiratory syndrome. Lancet 2004; 363(9422):1699-700. doi: 10.1016/s0140-6736(04)16255-7 [Crossref] [ Google Scholar]
- Bavelloni A, Piazzi M, Raffini M, Faenza I, Blalock WL. Prohibitin 2: at a communications crossroads. IUBMB Life 2015; 67(4):239-54. doi: 10.1002/iub.1366 [Crossref] [ Google Scholar]
- Drosten C, Seilmaier M, Corman VM, Hartmann W, Scheible G, Sack S. Clinical features and virological analysis of a case of Middle East respiratory syndrome coronavirus infection. Lancet Infect Dis 2013; 13(9):745-51. doi: 10.1016/s1473-3099(13)70154-3 [Crossref] [ Google Scholar]
- Lai MY, Cheng PK, Lim WW. Survival of severe acute respiratory syndrome coronavirus. Clin Infect Dis 2005; 41(7):e67-71. doi: 10.1086/433186 [Crossref] [ Google Scholar]
- Casanova L, Rutala WA, Weber DJ, Sobsey MD. Survival of surrogate coronaviruses in water. Water Res 2009; 43(7):1893-8. doi: 10.1016/j.watres.2009.02.002 [Crossref] [ Google Scholar]
- Strasser J. Survival and Sodium Hypochlorite Disinfection of Potential Ebola Virus Surrogates MS2, PhiX-174, and Phi6 in a Conservative Matrix of raw Hospital Sewage and Human Fecal Waste. University of North Carolina at Chapel Hill; 2017. 10.17615/td9b-zv32.
- Bibby K, Fischer RJ, Casson LW, Stachler E, Haas CN, Munster VJ. Persistence of Ebola virus in sterilized wastewater. Environ Sci Technol Lett 2015; 2(9):245-9. doi: 10.1021/acs.estlett.5b00193 [Crossref] [ Google Scholar]
- Bibby K, Fischer RJ, Casson LW, de Carvalho NA, Haas CN, Munster VJ. Disinfection of Ebola virus in sterilized municipal wastewater. PLoS Negl Trop Dis 2017; 11(2):e0005299. doi: 10.1371/journal.pntd.0005299 [Crossref] [ Google Scholar]
- Chughtai AA, Barnes M, Macintyre CR. Persistence of Ebola virus in various body fluids during convalescence: evidence and implications for disease transmission and control. Epidemiol Infect 2016; 144(8):1652-60. doi: 10.1017/s0950268816000054 [Crossref] [ Google Scholar]
- Duan SM, Zhao XS, Wen RF, Huang JJ, Pi GH, Zhang SX. Stability of SARS coronavirus in human specimens and environment and its sensitivity to heating and UV irradiation. Biomed Environ Sci 2003; 16(3):246-55. [ Google Scholar]
- Wolff MH, Sattar SA, Adegbunrin O, Tetro J. Environmental survival and microbicide inactivation of coronaviruses. In: Schmidt A, Wolff MH, Weber O, eds. Coronaviruses with Special Emphasis on First Insights Concerning SARS. Springer; 2005. p. 201-12. 10.1007/3-7643-7339-3_10.
- Piercy TJ, Smither SJ, Steward JA, Eastaugh L, Lever MS. The survival of filoviruses in liquids, on solid substrates and in a dynamic aerosol. J Appl Microbiol 2010; 109(5):1531-9. doi: 10.1111/j.1365-2672.2010.04778.x [Crossref] [ Google Scholar]
- Ahmed W, Angel N, Edson J, Bibby K, Bivins A, O’Brien JW. First confirmed detection of SARS-CoV-2 in untreated wastewater in Australia: a proof of concept for the wastewater surveillance of COVID-19 in the community. Sci Total Environ 2020; 728:138764. doi: 10.1016/j.scitotenv.2020.138764 [Crossref] [ Google Scholar]
- Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H. First case of 2019 novel coronavirus in the United States. N Engl J Med 2020; 382(10):929-36. doi: 10.1056/NEJMoa2001191 [Crossref] [ Google Scholar]
- Tang A, Tong ZD, Wang HL, Dai YX, Li KF, Liu JN. Detection of novel coronavirus by RT-PCR in stool specimen from asymptomatic child, China. Emerg Infect Dis 2020; 26(6):1337-9. doi: 10.3201/eid2606.200301 [Crossref] [ Google Scholar]
- Wölfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Müller MA. Virological assessment of hospitalized patients with COVID-2019. Nature 2020; 581(7809):465-9. doi: 10.1038/s41586-020-2196-x [Crossref] [ Google Scholar]
- Wang J, Feng H, Zhang S, Ni Z, Ni L, Chen Y. SARS-CoV-2 RNA detection of hospital isolation wards hygiene monitoring during the coronavirus disease 2019 outbreak in a Chinese hospital. Int J Infect Dis 2020; 94:103-6. doi: 10.1016/j.ijid.2020.04.024 [Crossref] [ Google Scholar]
- Hart OE, Halden RU. Computational analysis of SARS-CoV-2/COVID-19 surveillance by wastewater-based epidemiology locally and globally: feasibility, economy, opportunities and challenges. Sci Total Environ 2020; 730:138875. doi: 10.1016/j.scitotenv.2020.138875 [Crossref] [ Google Scholar]
- Lodder W, de Roda Husman AM. SARS-CoV-2 in wastewater: potential health risk, but also data source. Lancet Gastroenterol Hepatol 2020; 5(6):533-4. doi: 10.1016/s2468-1253(20)30087-x [Crossref] [ Google Scholar]
- La Rosa G, Iaconelli M, Mancini P, Bonanno Ferraro G, Veneri C, Bonadonna L. First detection of SARS-CoV-2 in untreated wastewaters in Italy. Sci Total Environ 2020; 736:139652. doi: 10.1016/j.scitotenv.2020.139652 [Crossref] [ Google Scholar]
- Rimoldi SG, Stefani F, Gigantiello A, Polesello S, Comandatore F, Mileto D. Presence and infectivity of SARS-CoV-2 virus in wastewaters and rivers. Sci Total Environ 2020; 744:140911. doi: 10.1016/j.scitotenv.2020.140911 [Crossref] [ Google Scholar]
- Xu Y, Li X, Zhu B, Liang H, Fang C, Gong Y. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med 2020; 26(4):502-5. doi: 10.1038/s41591-020-0817-4 [Crossref] [ Google Scholar]
- Singer A, Wray R. Detection and survival of SARS-coronavirus in human stool, urine, wastewater and sludge. Preprints [Preprint]. June 18 2020. Available from: https://www.preprints.org/manuscript/202006.0216/v2.
- Wu F, Zhang J, Xiao A, Gu X, Lee WL, Armas F. SARS-CoV-2 titers in wastewater are higher than expected from clinically confirmed cases. mSystems 2020; 5(4):e00614-20. doi: 10.1128/mSystems.00614-20 [Crossref] [ Google Scholar]
- Randazzo W, Truchado P, Cuevas-Ferrando E, Simón P, Allende A, Sánchez G. SARS-CoV-2 RNA in wastewater anticipated COVID-19 occurrence in a low prevalence area. Water Res 2020; 181:115942. doi: 10.1016/j.watres.2020.115942 [Crossref] [ Google Scholar]
- Kocamemi BA, Kurt H, Hacıoglu S, Yaralı C, Saatci AM, Pakdemirli B. First data-set on SARS-CoV-2 detection for Istanbul wastewaters in Turkey. medRxiv [Preprint]. May 6, 2020. Available from: https://www.medrxiv.org/content/10.1101/2020.05.03.20089417v1.
- Ahmed F, Islam MA, Kumar M, Hossain M, Bhattacharya P, Islam MT. First detection of SARS-CoV-2 genetic material in the vicinity of COVID-19 isolation Centre in Bangladesh: variation along the sewer network. Sci Total Environ 2021; 776:145724. doi: 10.1016/j.scitotenv.2021.145724 [Crossref] [ Google Scholar]
- Wurtzer S, Marechal V, Mouchel J, Maday Y, Teyssou R, Richard E, et al. Evaluation of lockdown impact on SARS-CoV-2 dynamics through viral genome quantification in Paris wastewaters. medRxiv [Preprint]. May 6, 2020. Available from: https://www.medrxiv.org/content/10.1101/2020.04.12.20062679v2.
- Medema G, Heijnen L, Elsinga G, Italiaander R, Brouwer A. Presence of SARS-coronavirus-2 RNA in sewage and correlation with reported COVID-19 prevalence in the early stage of the epidemic in the Netherlands. Environ Sci Technol Lett 2020; 7(7):511-6. doi: 10.1021/acs.estlett.0c00357 [Crossref] [ Google Scholar]
- Bivins A, Greaves J, Fischer R, Yinda KC, Ahmed W, Kitajima M. Persistence of SARS-CoV-2 in water and wastewater. Environ Sci Technol Lett 2020; 7(12):937-42. doi: 10.1021/acs.estlett.0c00730 [Crossref] [ Google Scholar]
- Buscarini E, Manfredi G, Brambilla G, Menozzi F, Londoni C, Alicante S. GI symptoms as early signs of COVID-19 in hospitalised Italian patients. Gut 2020; 69(8):1547-8. doi: 10.1136/gutjnl-2020-321434 [Crossref] [ Google Scholar]
- Mesoraca A, Margiotti K, Viola A, Cima A, Sparacino D, Giorlandino C. Evaluation of SARS-CoV-2 viral RNA in fecal samples. Virol J 2020; 17(1):86. doi: 10.1186/s12985-020-01359-1 [Crossref] [ Google Scholar]
- Du W, Yu J, Liu X, Chen H, Lin L, Li Q. Persistence of SARS-CoV-2 virus RNA in feces: a case series of children. J Infect Public Health 2020; 13(7):926-31. doi: 10.1016/j.jiph.2020.05.025 [Crossref] [ Google Scholar]
- Zhang HW, Yu J, Xu HJ, Lei Y, Pu ZH, Dai WC. Corona virus international public health emergencies: implications for radiology management. Acad Radiol 2020; 27(4):463-7. doi: 10.1016/j.acra.2020.02.003 [Crossref] [ Google Scholar]
- Ahmed W, Bertsch PM, Bibby K, Haramoto E, Hewitt J, Huygens F. Decay of SARS-CoV-2 and surrogate murine hepatitis virus RNA in untreated wastewater to inform application in wastewater-based epidemiology. Environ Res 2020; 191:110092. doi: 10.1016/j.envres.2020.110092 [Crossref] [ Google Scholar]
- Chen Y, Chen L, Deng Q, Zhang G, Wu K, Ni L. The presence of SARS-CoV-2 RNA in the feces of COVID-19 patients. J Med Virol 2020; 92(7):833-40. doi: 10.1002/jmv.25825 [Crossref] [ Google Scholar]
- Zhang HW, Yu J, Xu HJ, Lei Y, Pu ZH, Dai WC. Corona virus international public health emergencies: implications for radiology management. Acad Radiol 2020; 27(4):463-7. doi: 10.1016/j.acra.2020.02.003 [Crossref] [ Google Scholar]
- Xing Y, Ni W, Wu Q, Li W, Li G, Tong J, et al. Prolonged presence of SARS-CoV-2 in feces of pediatric patients during the convalescent phase. medRxiv [Preprint]. March 13, 2020. Available from: https://www.medrxiv.org/content/10.1101/2020.03.11.20033159v1.
- Kim JY, Ko JH, Kim Y, Kim YJ, Kim JM, Chung YS. Viral load kinetics of SARS-CoV-2 infection in first two patients in Korea. J Korean Med Sci 2020; 35(7):e86. doi: 10.3346/jkms.2020.35.e86 [Crossref] [ Google Scholar]
- Ling Y, Xu SB, Lin YX, Tian D, Zhu ZQ, Dai FH. Persistence and clearance of viral RNA in 2019 novel coronavirus disease rehabilitation patients. Chin Med J (Engl) 2020; 133(9):1039-43. doi: 10.1097/cm9.0000000000000774 [Crossref] [ Google Scholar]
- Lo IL, Lio CF, Cheong HH, Lei CI, Cheong TH, Zhong X. Evaluation of SARS-CoV-2 RNA shedding in clinical specimens and clinical characteristics of 10 patients with COVID-19 in Macau. Int J Biol Sci 2020; 16(10):1698-707. doi: 10.7150/ijbs.45357 [Crossref] [ Google Scholar]
- Zhang N, Gong Y, Meng F, Bi Y, Yang P, Wang F. Virus shedding patterns in nasopharyngeal and fecal specimens of COVID-19 patients. medRxiv [Preprint]. March 30, 2020. Available from: https://www.medrxiv.org/content/10.1101/2020.03.28.20043059v1.
- Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology 2020;158(6):1831-3.e3. 10.1053/j.gastro.2020.02.055.