Avicenna J Environ Health Eng. 7(2):92-96.
doi: 10.34172/ajehe.2020.14
Original Article
Bacterial Contamination of Mobile Phones Carried by Medical Staff in Maternity, Neonatal, and ICU Wards of Shahid Beheshti and Imam Sajjad Hospitals in Yasuj
Maryam Heydari 1, 2, Fatemeh Ehsani 1, 2, Mohsen Naghmachi 1, Mehdi Salari 3, Mohammad Noorisepehr 4, Maryam Moradnia 5, Mohammad Darvishmotevalli 4, Asiyeh Bazmeh 6, 7, *
Author information:
1Department of Environmental Health Engineering, School of Health, Yasuj University of Medical Sciences, Yasuj, Iran
2Student Research Committee, School of Health, Yasuj University of Medical Sciences, Yasuj, Iran
3Department of Environmental Health Engineering, School of Health, Hamadan University of Medical Sciences, Hamadan, Iran
4Research Center for Health, Safety and Environment (RCHSE), Alborz University of Medical Sciences, Karaj, Iran
5Student Research Committee, Department of Environmental Health Engineering, School of Health, Isfahan University of Medical Sciences, Isfahan, Iran
6Department of Environmental Health Engineering, School of Health, Isfahan University of Medical Sciences, Isfahan, Iran
7Student Research Committee, School of Health, Isfahan University of Medical Sciences, Isfahan, Iran
Abstract
The use of mobile phones by healthcare personnel, doctors, patients, and patients’ companions are unavoidable in health centers, especially in hospitals. Besides being rarely clean, the mobile phone is a potential reservoir of disease and pathogens and hospital infections on bedside of hospitalized patients. In this study, the microbial contamination of mobile phones and potential of transmitting infections and their antibiotic resistance pattern were investigated. In this descriptive cross-sectional study, a questionnaire was prepared to assess the importance of maternity, neonatal, and intensive care unit (ICU) staff attention to how to use and clean the cell phones in terms of valid sources. Samples were taken from 116 cell phones using a sterile swab. The standard plate count was used to detect the existing bacteria, and the antimicrobial resistance patterns of isolated bacteria were determined by standard methods. The microbial culture experiments indicated that 107 cell phones had microbial contamination, accounting for 92.24% of mobile phones. From 132 isolated strains, 115 strains (87.12%) were gram-positive while 17 were Gram-negative (12.88%). Furthermore, 67 (57.76%), 9 (7.7%), 4 (3.45%), 10 (8.62%), 12 (10.35%), 22 (19%), and 8 (6.9%) strains were coagulase-negative staphylococci, Pseudomonas aeruginosa, Staphylococcus aureus, Corynebacterium, Bacillus, Streptococcus, and Escherichia coli, respectively. The results of this study indicated that cell phones were contaminated with different types of bacteria, and that all species isolated partially played an important role in the development of hospital-acquired and opportunistic infections. Therefore, continuous disinfection of mobile phones and non-use or limited use of them in the hospitals are recommended.
Keywords: Mobile phone, Bacterial contamination, Hospital personnel, Microbial resistance, Antibiogram
Copyright and License Information
© 2020 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
1. Introduction
Microorganisms are scattered everywhere. Soil, water, air, human body, animals, different surfaces, all have microbial contamination. If these germs grow and spread, they can easily cause microbial contamination, poisoning, and infection (1). Hospital-acquired infection or nosocomial infection is an infection that afflicts the patient in a hospital. Microbial contamination leading to hospital infections is an important problem in all modern hospitals (2). In industrialized countries, about 5% to 10% of the patients get nosocomial infection in hospital and this number rises to about 25% in developing countries (3). With respect to the World Health Organization (WHO) in the Middle East region, where Iran is located, about 10 to 15% of the patients suffer from hospital infections, with an infection rate of 8% in Iran (4). The most effective, low-cost, and optimal way to fight infection at any time and place is to prevent it (5).This infection may be transmitted to patients by bacteria through hand-infected healthcare workers-associated infection and inanimate surfaces, and can result in high mortality rate (6). Medical devices (endotracheal tube, laryngoscope and tracheostomy tube) and surfaces of thermometers, speakers, cell phones, and even toys in the pediatric department could easily transmit the infection to patients (6). Ubiquitous objects are easily infected by microorganisms in the hospital environment. Due to the large usage of mobile phones in different places, including hospitals, this device can be considered a suitable position for deploying microorganisms in hospitals, especially when the humidity and temperature are high (7). As thousands of microbes can survive in cell phones, every inch of the cell phones can spread and transmit infectious diseases in the hospital environment because of their frequent contact with hands and face (8). Given the extensive use of mobile phones in the community, microbial contamination of mobile phones is also important for doctors, the operating room staff, and all healthcare providers (6). Unlike hands that are usually washed, disinfection and constant cleaning of mobile phones are awkward and usually overlooked (10). Cell phones are often used by patients, visitors, and healthcare workers in the hospital environment (10). Moreover, communication technology in this device has resulted in developing new approaches for providing healthcare and improving the speed and quality of regular communication between medical science and medical staff (11). The hospitals, operating rooms, and neonatal departments of the hospitals should be free from any pathogenic bacteria, and the number of saprophytic microorganisms should not exceed 20 cfu (12). Infections caused by bacterial contamination of mobile phones that are used in maternity hospitals, ICU, and neonatal areas during or after work without sterilization can stimulate taking the necessary measures for controlling infection and reducing environmental contamination in hospitals (11). The purposes of this study were to investigate the cellphone contamination with bacterial agents causing hospital infections, and also their antibiotic pattern in three wards, namely maternity, neonatal, and ICU wards.
2. Materials and Methods
2.1. Sampling Method
Data were to be collected from three public hospitals affiliated to Yasuj University of Medical Sciences. To this end, a letter was sent to the Hospital Officials from the vice-chancellor and the Head of the Research Institute to collect microbial samples from the desired sections. The samples were taken from a square centimeter on staff cell phone who were employed in different wards. Taking into account all the personnel of the 3 wards of Shahid Beheshti and Imam Sajjad hospitals, the samples consisted of 116 cell phones of physicians, nurses, and midwives in maternity sections, neonatal, and intensive care unit (ICU) wards of Shahid Beheshti and Imam Sajjad Hospitals in Yasuj. Sterilized swabs were used for sampling, and the samples were then placed in Trypticase soy broth media. Separately, a square centimeter of mobile surface was sampled. This sample was put in 1 mL of normal saline, which was used to count the microorganisms. By maintaining the correct temperature with thermometer in cold boxes, the samples were transferred to the Microbiology Laboratory of Yasouj University of Medical Sciences.
2.2. Bacterial Count
The specimen used for counting was cultivated on Nutrient Agar using the standard plate count method. After incubation for 24 hours at 37°C, counting was accomplished by a colony counter (9,13).
2.3. Isolation and Detection of Bacteria
Twenty-four hours past the incubation of the samples at 37°C, a portion of the samples were cultured on Eosin Methylene Blue (EMB) agar and another portion on a blood agar medium, and again incubated at 37°C, and afterward, they were stored for 24 hours (2,4). After growth, different colonies were applied to gram staining in terms of shape, color, and margin, and the hemolysis was determined, then appropriate tests were employed to detect the bacteria. Different environments for gram negativities were EMB agar, Triple Sugar Iron (TSI) agar, SIM medium, Simon’s Citrate agar, Urea agar, and Muller Hinton agar, and differential media were used to detect Blood agar, Löffler’s medium, DNase agar, and bile-esculin agar (14,15). The tests for identifying gram-negative and gram-positive bacteria were included in oxidase, catalase, and nuclease, sensitivity to bacitracin, novobiocin, and optochin (4,10).
2.4. Study of Microbial Resistance Pattern
To assess susceptibility of isolated bacteria to antibiotics, an antibiogram test was performed using a disk diffusion method with respect to the Clinical and Laboratory Standards Institute (CLSI) guidelines. The results were analyzed by descriptive statistical tests using SPSS software.
3. Results and Discussion
For this study, 116 samples were collected from mobile phones belonging to the personnel at maternity, neonatal, and ICU wards. The personnel were 6 physician and medical students, 9 practical nurses, and 7 service providers, 74 nurses, and 20 midwives. The differential tests indicated that 92.24% of the cell phones were positive for culture and microbial contamination. Totally, 132 strains of microbial isolates were isolated from mobile phones, and were diagnosed from each other by differential tests of gram-negative and gram-positive bacteria. From these strains, 115 (87.12%) were gram positive and 17 were gram negative (12.88%). The percentage of bacteria isolated from mobile phone surfaces BY GRAM STAINING IS SHOWN in Fig. 1. The isolated strains were as follows: 67 strains of Staphylococcus coagulase (57.76%), 9 strains of Pseudomonas aeruginosa (7.7%), 4 strains of Staphylococcus aureus (3.45%), 10 strains of Corynebacterium (8.62%), 12 strains of Bacillus (10.35%), 22 strains of Streptococcus (19%), and 8 strains of E. coli (6.9%). Fig. 2 shows the percentage and genus of bacteria isolated from mobile phone surfaces. The results of bacterial counts per square centimeter (standard level) of each mobile phone indicated that the average bacterial count with a standard deviation was 88 ± 6.7. To study the conventional antibiotic susceptibility, antibiogram test was done for 132 strains using disk diffusion method and with respect to the CLSI instructions. It was found that 83 strains were resistant to clindamycin (62.88%), 64 were resistant to erythromycin (48.5%), 92 were resistant to ceftazidime (69.7%), 96 were resistant to ampicillin (72.7%), 82 were resistant to penicillin (62.12%), 68 were resistant to tetracycline (51.5%), 36 were resistant to chloramphenicol (27.27%), and 23 were resistant to ampicillin (17.43%). Table 1 represents the comparison of microbial resistance of strains isolated from mobile phone surfaces to different antibiotics. In addition to the tests, a questionnaire was also prepared to explore the habits of the staff and their care and attention to sanitizing the mobile phones. It was found that 97.41% of the personnel were directly involved with patients, and 85.75% of the staff used their mobile phones while they were going to the hospital, and 51.72% carried their mobile devices in their pockets and 29.32% used their mobile phones during contact with the patients.
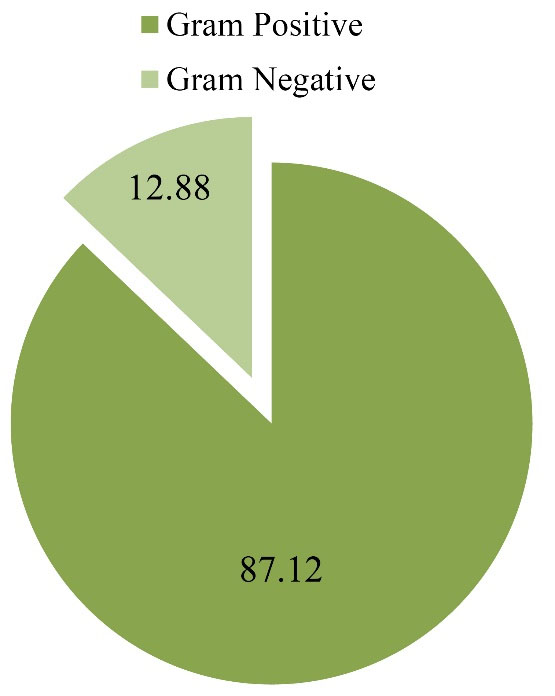
Figure 1.
Percentage of Bacteria Isolated From Mobile Phones by Gram Staining.
.
Percentage of Bacteria Isolated From Mobile Phones by Gram Staining.
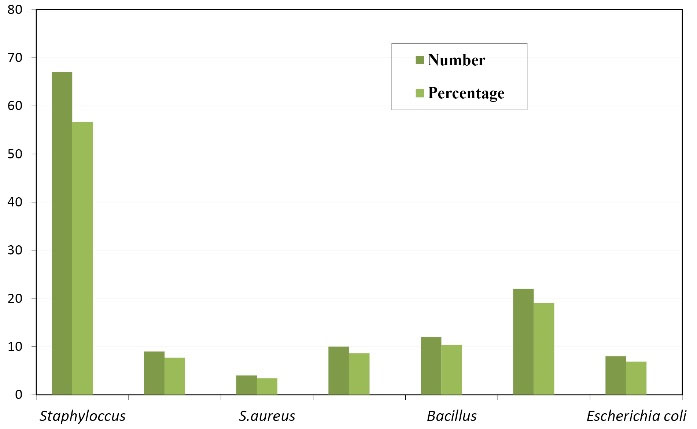
Figure 2.
Number and Genus of Bacteria Isolated From Mobile Phone Surfaces.
.
Number and Genus of Bacteria Isolated From Mobile Phone Surfaces.
Table 1.
Antibiotic Resistance of Strains Isolated From Mobile Phones
|
Antibiotics
|
Number of Resistant Spices
|
Percentage of Resistant Spices
|
| Clindamycin |
83 |
62,88 |
| Erythromycin |
64 |
48.5 |
| Ceftazidime |
92 |
69.7 |
| Ampicillin |
82 |
62.12 |
| Penicillin |
96 |
72.7 |
| Tetracycline |
68 |
51.5 |
| Chloramphenicol |
36 |
27.27 |
| Imipenem |
23 |
17.43 |
Equipment and devices present in hospital environment are easily contaminated with microorganisms. Due to the extensive usage of mobile phones in various places, including hospitals, these devices can be considered a suitable platform for the deployment of microorganisms, especially when the humidity and temperature are high (7). Regarding the fact that every square inch of the cell phone contains thousands of microbes, cell phones can be a reservoir for spreading and transmitting the infectious diseases in the hospital environment due to their frequent contact with hands and face (8). As stated, after collecting the samples and doing microbial tests, the vast majority of mobile phones of hospital staff in the maternity, neonatal, and ICU wards were positive for bacteria. Gram-positive strains showed a significantly greater portion of the taken samples compared to gram-negative strains. In this study, resistance was observed to clindamycin, erythromycin, ceftazidime, ampicillin, penicillin, tetracycline, chloramphenicol, and imipenem. Staphylococcus causes a wide range of infections such as bacteremia, sepsis, skin infections, and other infections. At the moment, drug resistance among gram-positive Staphylococcus bacteria has caused many problems in the treatment of infections caused by this bacterium. The immune system of hospitalized patients is weakened due to the stress of illness and hospitalization; and measures such as insertion of venous catheters lead to susceptibility to various infections, and if hospital staff do not observe the hygiene of their hands and devices, infection with these germs occurs more often. For example, in some reports, coagulase-negative staphylococci have been one of the leading causes of urinary tract and nosocomial infections (16), blood infections in hospitalized patients, and immunosuppression (17). It has been also responsible for more than half of the intravenous catheter infections in the neonatal ward (18). In similar studies conducted in other countries, cell phone contamination has been also reported. For example, in Turkey, 94.5% of microbial contamination was found on mobile phones, from which 31.3% were gram-negative strains that were resistant to ceftazidime. Furthermore, methicillin-resistant S. aureus strains has extensively been reported. This study indicated that some cell phones were contaminated with major pathogens of the hospital (2). In another study, 62% of the contamination detected in mobile phones was with strains of Staphylococcus coagulase, S. aureus, Enterococcus faecalis, P. aeruginosa, and Klebsiella species, from which the highest prevalence belonged to S. aureus (10). Based on another study, despite disinfection of the cell phones with 70% isopropyl alcohol, contamination was found to be 40.62% (13). Yet in another study conducted in Iran, the contamination rate of mobile phones carried by health personnel was 56.62% and bacteria isolated in this study were S. aureus (56.52%), Bacillus species (25.26%), and E. coli (17.4%) (19). In another study, 95.66% of the isolated bacterial species were coagulase-negative staphylococci, gram positive bacilli, Klebsiella, and E. coli (20). As can be observed, the results of the present study are almost consistent with the results of other studies. The difference was observed in bacterial species and percentages, which could be attributed to the geographical and environmental differences. And what is more, because of frequent contact of mobile phone with skin and with other items in the environment, majority of bacterial species on mobile phone surfaces are affected by the natural flora of the individual’s skin or environment. In this study, the coagulase negative stapyhlococci had have more amount compared with other microorganism. Antibiotic resistance patterns are also different in different places because of the presence of common strains in the area and usage of antibiotics, and also the type of antibiotics used. In this study, according to the data from the questionnaires, a number of people had skin and respiratory diseases. A reasonable percentage of people keep their cell phones in their pockets or keep them in touch with their hands. From all the staff, those in contact with patients were in the majority, while 82.75% of them were using their cell phones while going to a ward, and 29.32% used their mobile phones when they were in contact with patient. In a study conducted on mobile phones of staff in Shahid Beheshti hospital, Iran (4), all of the subjects were using the cell phone in the hospital, from which, 48% used their phones while they were taking care of patient, and 34% kept their phones in their pockets. In general, considering the need of community members and health care personnel for using mobile phones, it can be concluded that method of use or using this device during work is in contrast with instructions, while its use is unfortunately common. Few people care about disinfecting their mobile devices before working. Mobile contamination sources include normal skin flora, Infection agents, and environmental pollutants that are of great importance in therapeutic environments due to the presence of antibiotic-resistant strains which play an important role in the development of hospital-acquired infectious diseases. In this regard, cell phones have been turned into a potential reservoir for the transmission of hospital-acquired infectious agents. Accordingly, continuous cleaning the cell phones and not using mobile phones in hospital departments are strongly recommended.
4. Conclusion
According to the results of this study, as well as other similar studies, mobile phones are associated with different types of bacteria. The cell phones are frequently used by the staff in the hospital environment during the patient visits. It is possible that the staff touch their cell phones before visiting a patient; this can be considered as a source of hospital infection in hospitals. Hence, continuous cleaning the cell phones and not using the mobile phones in hospital departments are strongly recommended. Although it is necessary to demonstrate the direct relationship between hospital infections and transmission of these infections through cellphones and hands, it is notable that using mobile phones in internal wards of the hospital are not allowed. This study was done in two small-scale hospitals. It is suggested that more extensive studies be carried out in the medical and surgical wards of hospitals. It is also recommended that in future studies, more basic factors such as sampling from the hands of hospital staff, or examination of how employees disinfect their phones should be considered in order to further clarify the situation.
Conflict of Interest Disclosures
The authors declare no conflict of interests regarding this study.
Ethical Statement
Ethical approval for this study was provided by the Ethics Board of the Vice-Chancellor for Research and Technology of Yasuj University of Medical Sciences (Code of ethics: 93.12.03.15).
Acknowledgments
Our sincere gratitude goes to the Vice-Chancellor for Research and Technology of Yasuj University of Medical Sciences for financial support of this research.
References
- Brooks GF, Jawetz E, Melnick JL, Adelberg EA, Carroll KC. Jawetz, Melnick & Adelberg’s Medical Microbiology. 26th ed. New York: McGraw-Hill; 2013.
- Ulger F, Esen S, Dilek A, Yanik K, Gunaydin M, Leblebicioglu H. Are we aware how contaminated our mobile phones with nosocomial pathogens?. Ann Clin Microbiol Antimicrob 2009; 8:7. doi: 10.1186/1476-0711-8-7 [Crossref] [ Google Scholar]
- Soleymani asl H, Afhami Sh. Prevention and control of nosocomial infections. 2nd Ed. Tamirzadeh; 2008. p. 831.
- Alighardashi M, Aeini M, Aeinian F, Mohamadi H. The amount and type of microbial contamination on cell phones of medical staff in Shahid Beheshti hospital, Hamadan, Iran. Journal of Health System Research 2011; 7(6):533. [ Google Scholar]
- Mousavi SM, Dargahi H, Hasibi M, Mokhtari Z, Shaham G. Evaluation of safety standards in operating rooms of Tehran University of Medical Sciences (TUMS) hospitals in 2010. Payavard Salamat 2011; 5(2):10-7. [ Google Scholar]
- Badr RI, Badr HI, Ali NM. Mobile phones and nosocomial infections. Int J Infect Control 2012; 8(2):1-5. doi: 10.3396/ijic.v8i2.9933 [Crossref] [ Google Scholar]
- Srikanth P, Ezhil R, Suchitra S, Anandhi I, Maheswari U, Kalyani J. The mobile phone in a tropical setting - emerging threat for infection control. 13th International Congress on Infectious Diseases Abstracts; 2015. p. 367.
- Suganya S, Sumathy JH. Isolation and identification of bacteria from covered and uncovered mobile phones. Int J Environ Sci 2012; 3(1):44-54. doi: 10.6088/ijes.2012030131006 [Crossref] [ Google Scholar]
- Zobeyri M, Karami Matin B. Determining of microbial contamination and its related factors in hands of ICU staff in the hospitals of Kermanshah (2002). J Kermanshah Univ Med Sci 2005; 9(2):52-7. [ Google Scholar]
- Akinyemi KO, Atapu AD, Adetona OO, Coker AO. The potential role of mobile phones in the spread of bacterial infections. J Infect Dev Ctries 2009; 3(8):628-32. doi: 10.3855/jidc.556 [Crossref] [ Google Scholar]
- Brady RR, Verran J, Damani NN, Gibb AP. Review of mobile communication devices as potential reservoirs of nosocomial pathogens. J Hosp Infect 2009; 71(4):295-300. doi: 10.1016/j.jhin.2008.12.009 [Crossref] [ Google Scholar]
- Laripour M, Sultani M. A review on microbial contamination of air in hospital infections and its prevention methods. Journal of Islamic Azad University 2009; 2(5):57-65. [ Google Scholar]
- Arora U, Devi P, Chadha A, Malhotra S. Cellphones a modern stayhouse for bacterial pathogens. JK Sci 2009; 11(3):127-9. [ Google Scholar]
- Zarinfar N, Akbari M, Sharafkhah M. Evaluation of antibiotic resistance profile of gram-negative bacteria isolated from inpatients of an academic and non-academic hospitals in the Arak, Iran 2011-2012. J Arak Uni Med Sci 2013; 16(79):47-60. [ Google Scholar]
- Ramazanzadeh R, Moradi GH, Zandi S, Mohammaadi S, Rouhi S, Pourzere M. Evaluation of antibiotic resistance of gram–negative bacteria isolated from patients in different of Tohid and Besat hospitals in Sanandaj. Journal of Scientific Researchers 2017; 14(3):11-9. [ Google Scholar]
- Amin M, Mehdinezhad M, Pourdangchi Z. Study of bacteria isolated from urinary tract infections and determination of their susceptibility to antibiotics. Jundishapur J Microbiol 2009; 2(3):118-23. [ Google Scholar]
- Daneshi MM, Sarookhani MR, Habibi M. Colonization rate of intravascular catheters and catheter related bacteremia in neonatal intensive care unit of Qods hospital, Qazvin (2005). J Qazvin Univ Med Sci 2007; 11(3):9-13. [ Google Scholar]
- Behrman RE, Kliegman RM, Jenson HB. Nelson Textbook of Pediatrics. 17th ed. Philadelphia: W.B. Saunders; 2004. p. 861-7.
- Masoomi A. National Guideline to Hospital Care System, Publication of the Ministry of Health and Medical Education, Center for Disease Control, 2005. p. 73-111.
- Sedighi I, Alikhani MY, Ramezani S, Nazari M, Mozaffari Nejad AS. Bacterial contamination of mobile phones of health care providers in a teaching hospital in Hamadan province, Iran. Arch Clin Infect Dis 2015; 10(2):e22104. doi: 10.5812/archcid.10(2)2015.22104 [Crossref] [ Google Scholar]