Avicenna J Environ Health Eng. 6(2):119-123.
doi: 10.34172/ajehe.2019.16
Review Article
The Potential Effectiveness of Probiotic-Based Sanitation Procedures in Nosocomial Infection Control: A Review Article
Masoumeh Moghaddam Arjmand * 
Author information:
Department of Environmental Health Engineering, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran
Abstract
The sanitation of the hospital environment for the purpose of preventing the transmission of nosocomial infections has a major role in reducing the infection of hospitalized patients with the bacteria living on hospital surfaces. The excessive use of chemical detergents in recent decades has led to microbial resistance in nosocomial infectious bacteria. Researchers’ attention has therefore been drawn to the use of probiotics for disinfecting hospital surfaces. The present study was conducted to assess the potential effectiveness of probiotic products in controlling the contamination of inert surfaces in the environment and medical instruments in health centers and investigate the claim that the antagonistic property of probiotic microorganisms offers an effective method for controlling nosocomial infections and a suitable alternative to conventional disinfection methods. A search was carried out for relevant articles published from 2000 to 2018 in databases including ISI, PubMed, Scopus, EMBASE, and Google Scholar, using the keywords "nosocomial infections", "disinfection", "sanitation", "probiotics" and "infected surfaces". The articles published from 2000 to 2018 confirmed the greater effectiveness of probiotic disinfection (by up to 90%) compared to conventional chemical disinfection in controlling nosocomial infections. Nevertheless, more extensive studies are needed on probiotics to determine the possibility of replacing good bacteria with bad bacteria in future decades.
Keywords: Nosocomial infection, Disinfection, Probiotic, Infected surfaces, Pathogens
Copyright and License Information
© 2019 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
1. Introduction
Contaminated surfaces in hospitals provide an important source for transmission of health care-associated pathogens (1). Therefore, the use of disinfectants has a major role in the management of nosocomial infections. As a huge challenge throughout the world, nosocomial infections threaten the health of 15% of hospitalized patients (2,3). Pathogens including vancomycin-resistant Enterococcus, methicillin-resistant Staphylococcus aureus, Norovirus, Clostridium difficile, and multidrug-resistant gram-negative bacteria (MDR) can survive in the hospital environment for days and months and act as a source of spreading infection (4-6). Conventional sanitation based on the use of chemicals not only is ineffective in preventing the re-infection of surfaces but also produces multidrug-resistant microbial strains. The theory of probiotic-based improvement was formed and probiotic microorganisms were first introduced by Kramer et al, who pointed out their antagonistic effect on the proliferation of pathogens on hospital surfaces (3). By producing the extracellular polysaccharide matrix, Staphylococcus aureus and Escherichia coli adhere to inert surfaces and produce biofilm (7). This biofilm formation enables microorganisms to benefit from survival against their planktonic (free-floating) rivals and provides an optimal environment for the growth, proliferation, gene transfer, and the microbial population development. The proximity of rival species can have an antagonistic effect on the formation of biofilm (8). Lactobacillus species can produce amphipathic molecules called bio-surfactant, which have anti-adhesion properties against pathogenic microbes (9,10). The extensive use of chemical disinfectants not only produces disinfectant-resistant microbial strains but also makes them resistant against antibiotics. According to a recent report, using chlorhexidine leads to the emergence of multidrug-resistant gram-negative bacteria (MDR-GNB) against colistin. This antibiotic was used until 2016 as the drug of last resort for the treatment of infections caused by MDR-GNB (11). The potential to cause microbial resistance is a highly undesirable side-effect of chemical detergents, and the spread of pathogens is responsible for a large part of nosocomial infections (12,13). Self-disinfecting method can be proposed as an alternative method in which hospital surfaces are smeared with a bactericidal agent using silver and copper. This method is expensive and not suitable for all surfaces (14). The issue of minimizing the risk of nosocomial infection and preventing the increase in drug resistance has turned the attention of researchers to the management of “hospital environment sanitation” instead of “patients’ physical health” (15,16). The present article aims to review the potential effectiveness of bio-surfactants in controlling nosocomial infections in studies conducted from 2000 to 2018.
2. Materials and Methods
2.1. Study Objective
The present study aimed to review articles published from 2000 to 2018 to find evidence in favor of the claim that probiotics have the required effectiveness for controlling nosocomial infections.
2.2. Study Strategy
Published literature was retrieved through a search using the words (MeSH was applied to select appropriate keywords) “microbial infection”, “infection control”, “disinfectant”, “probiotic organisms”, “bio-surfactant”, “nosocomial infections” and “sanitation” in databases including PubMed, EMBASE, ISI, and Google Scholar (2000-2018) (Fig. 1).
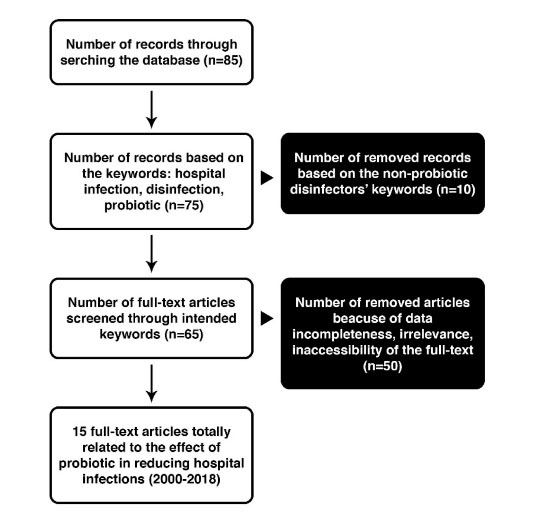
Figure 1.
Flow Chart of Literature Review (2000-2018) of Included and Excluded Studies for Nosocomial Disinfection by Probiotics.
.
Flow Chart of Literature Review (2000-2018) of Included and Excluded Studies for Nosocomial Disinfection by Probiotics.
2.3. Article Inclusion Criteria and Data Extraction
First, the abstracts of all the retrieved papers were reviewed to select the relevant articles. Then, data were extracted by reviewing the full text of the selected articles. The data extraction criteria consisted of the type of experiment, results, type of probiotic and type of hospital organism.
3. Results and Discussion
Of the 65 articles retrieved, 15 were identified as relevant (Fig. 1). After printing out the full text of all these articles, the careful assessment of the data and results was carried out personally. Half of the experiments were in vitro experiments and the other half were field evidence. The Bacillus species made up a greater proportion of the probiotic bacteria. According to Table 1, the probiotic-based sanitation methods used in the experiments had been able to reduce pathogens on hospital surfaces about 50% to 100% more than conventional chemical methods.
Table 1.
The Effectiveness of Probiotic Bacteria in Reducing Hospital Pathogens
|
Method
|
Reference
|
Probiotics
|
Surfaces
|
Hospital Bacteria
|
Outcome
|
| In situ |
Caselli et al (2018) (17) |
PCHS (probiotic cleaning hygiene system) |
Floor, Sink, Footboard |
Staphylococcus spp., Enterobacteriaceae spp., Acinetobacter spp., Mycetes, Pseudomonas spp., Clostridium difficile
|
Over 83% reduction of surfaces pathogens |
| Commercial hatchery |
Graham et al (2018) (18) |
Bacillus subtilis
|
|
Staphylococcus, Pseudomonas, Escherichia coli
|
|
| In situ |
Caselli (2017) (19) |
Bacillus subtilis, Bacillus pumilus, Bacillus megaterium
|
Floor, Sink |
Common bacteria |
Over 90% reduction compared to the routine methods |
| In situ |
Caselliet al(2016) (20) |
Controlled pre-post interventional study |
|
Hospital bacteria |
Over 90% reduction compared to the routine methods |
| In vitro, in situ (opinion) |
Caselli et al (2016) (21) |
Bacillus subtilis, Bacillus pumilus, Bacillus megaterium
|
|
|
Over 90% reduction compared to the routine methods |
| In vitro |
Fanciet al (2015) (22) |
|
Floor, Washbasin, Desk |
Enterococcus faecalis, Candida albicans, Pseudomonas, Acinetobacter, Klebsiella pneumoniae
|
92.2%-99.9% bacterial reduction, 100% reduction of Pseudomonas, Acinetobacter |
| In vitro |
Vandini et al (2014) (23) |
Bacillus subtilis spp. spores |
Floor, Sink, Toilet |
Staphylococcus aureus Coliforms Pseudomonas spp. Candida spp.
|
Over 80% reduction of microbial load |
| In situ |
Vandini et al (2014) (24) |
Genus of bacillus |
Floor, Doors,Showers toilet, Windows sill, Sink (all made of stone, plastic, wood, glass, and metal) |
Coliforms, Staphylococcus aureus, Clostridium difficile, Candida albicans
|
50%-89% reduction in microbial load on the surfaces |
| In situ and in vitro |
Mazzacane et al (2014) (25) |
Genus of Bacillus, vegetative form and spore |
Toilet, Floor, Corridor floor |
Coliforms, Staphylococcus aureus, Candida albicans, Acinetobacter spp., Pseudomonas spp.
|
About 90% reduction in microbial cell |
| In vitro |
Walencke et al (2008) (26) |
Lactobacillus acidophilus
|
Floor |
Staphylococcus aureus, Staphylococcus epidermidis biofilm |
About 5%-56% reduction |
| In vitro |
Rodrigues et al (2006) (27) |
Streptococcus thermophilus
|
Silicon, Rubber |
Coliforms, Staphylococcus aureus, Candida albicans, Acinetobacter spp., Pseudomonas spp.
|
97% reduction in adhesion of bacterial cell |
| In vitro |
Rodrigues et al (2004) (28) |
Lactococcus lactis
|
Silicon, Rubber |
Staphylococcus aureus, Candida albicans, Staphylococcus epidermidis, Streptococcus salivarius
|
Adhesion of pathogenic bacteria |
| In vitro |
Rodrigueset al (2004) (29) |
Streptococcus thermophilus, Lactococcus lactis
|
Silicon, Rubber |
Staphylococcus aureus, Candida albicans, Staphylococcus epidermidis, Streptococcus salivarius
|
Significant decrease in the number of bacteria on the surface |
| In vitro |
Hoogmoed et al (30) |
Streptococcus mitis
|
Glass |
Streptococcus mutans
|
Release of biosurfactant by Streptococcus mitis and decrease in the number of s. mutans cells |
| In vitro |
Vander Mei et al (2000) (31) |
Lactobacillus spp., Streptococcus thermophilus
|
Silicon, Rubber |
Candida spp., Streptococcus spp., Staphylococcus spp.
|
Decrease in the number of pathogens on the surface |
It is a generally-accepted fact that some good bacteria are crucial and valuable for human health and can be effectively used in the prevention and treatment of infectious diseases (32). Fig. 2 shows the schematic plan of replacing pathogens with probiotic bacteria.
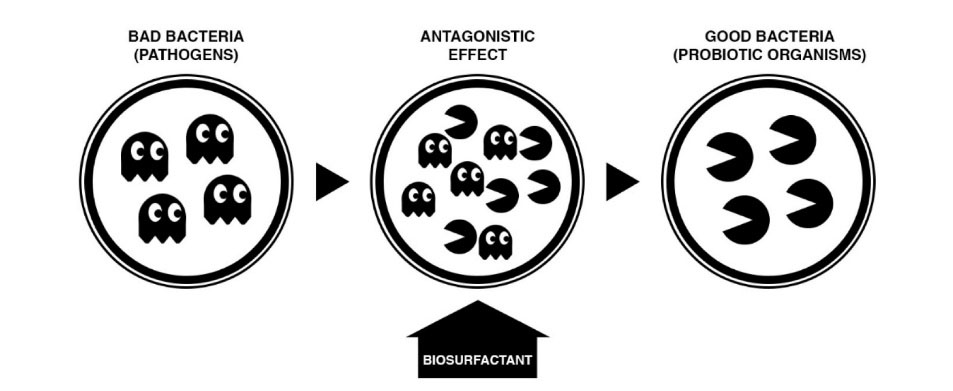
Figure 2.
The Schematic Plan of the Antagonistic Effect of Probiotic Bacteria on Pathogens Living on Hospital Surfaces and Medical Instruments.
.
The Schematic Plan of the Antagonistic Effect of Probiotic Bacteria on Pathogens Living on Hospital Surfaces and Medical Instruments.
Health care-associated infections are one of the serious problems concerning the safety of public health worldwide. As a challenge throughout the world, nosocomial infections threaten the health of 15% of hospitalized patients (33). It is well known that contaminated surfaces in hospitals act as reservoirs for the pathogenic bacteria, increasing the risk of infection (34). The extensive use of the traditional chemical disinfectants not only produces disinfectant-resistant microbial strains but also makes them resistant against antibiotics (11). The issue of minimizing the risk of nosocomial infection and the safety of public health has turned the attention of the researchers to the use of probiotic bacteria (17-31).
The results of the present review study show that despite the significant results reported, which generally confirm the effect of the probiotic-based sanitation method, a definitive answer cannot yet be given to the following questions: 1) How do probiotic microorganisms survive on inert surfaces and how long can they keep up and continue their dominance in competition with hospital pathogens? 2) To what extent are probiotics able to fight and act as antagonists against pathogenic microorganism growth? 3) How can we ensure the safety of probiotics and probiotic-containing detergents for consistent use in hospitals? 4) How can hospitalized patients’ health be promoted as a result of shifting from pathogens to probiotics? In other words, to what extent does replacing nosocomial pathogens with probiotics have a share in preventing dangerous pulmonary, gastric and urinary infections in patients? 5) Are probiotics and their products enough for inhibiting all microbial species? and 6) Is it possible for the epidemiology of nosocomial infections to be shifted toward microorganisms on which probiotics have no effect?
The in vitro experiments conducted on hydrophobic materials (such as glass) and hydrophilic materials (such as silicon) somewhat support the first question (35). The safety of using the probiotic-based sanitation method has been confirmed by the European Union Workshop (36), although several species of lactobacillus used in humans as probiotics have reportedly caused lactobacillus bacteremia (a very rare disease) in patients with serious underlying diseases (37). There has been a reduction in the frequency of nosocomial infections, diarrhea, colon infections (38), upper respiratory tract infections (39), and surgical site infections (40). The environmental parameters, such as humidity, temperature, and microbial flora, of different hospital units are regarded as factors affecting the disinfection of hospital surfaces and should therefore be considered in all antimicrobial processes.
This review study shows that a probiotic-based cleaning strategy is more effective (up to 90%) in reducing microbe, compared to a traditional chemical disinfectant. However, to develop a better understanding of the mechanism of the effectiveness of probiotics, further studies are needed.
4. Conclusion
The literature review (2000-2018) confirmed the greater effectiveness of probiotic disinfection (by up to 90%) compared to traditional chemical disinfection in controlling nosocomial infections. Since it is not possible to fully disinfect pathogens from all surfaces, nosocomial infections and drug-resistant pathogens can perhaps be controlled by relying on greater knowledge about the defects and shortcomings of the idea of using probiotics and by replacing “bad bacteria” with “good bacteria”. There is no easy way to remove microbes from surfaces. As a “green” alternative to chemical disinfectants, probiotics are biodegradable and environment-friendly. Using them is an innovative way to disinfect hospital environments effectively.
5. Acknowledgment
The review was performed by the sole author.
References
- Dancer SJ. Importance of the environment in meticillin-resistant Staphylococcus aureus acquisition: the case for hospital cleaning. Lancet Infect Dis 2008; 8(2):101-13. doi: 10.1016/s1473-3099(07)70241-4 [Crossref] [ Google Scholar]
- Dancer SJ. The role of environmental cleaning in the control of hospital-acquired infection. J Hosp Infect 2009; 73(4):378-85. doi: 10.1016/j.jhin.2009.03.030 [Crossref] [ Google Scholar]
- Kramer A, Schwebke I, Kampf G. How long do nosocomial pathogens persist on inanimate surfaces? a systematic review. BMC Infect Dis 2006; 6:130. doi: 10.1186/1471-2334-6-130 [Crossref] [ Google Scholar]
- Wagenvoort JH, Sluijsmans W, Penders RJ. Better environmental survival of outbreak vs sporadic MRSA isolates. J Hosp Infect 2000; 45(3):231-4. doi: 10.1053/jhin.2000.0757 [Crossref] [ Google Scholar]
- Chiang SR, Chuang YC, Tang HJ, Chen CC, Chen CH, Lee NY. Intratracheal colistin sulfate for BALB/c mice with early pneumonia caused by carbapenem-resistant Acinetobacter baumannii. Crit Care Med 2009; 37(9):2590-5. doi: 10.1097/CCM.0b013e3181a0f8e1 [Crossref] [ Google Scholar]
- Lawley TD, Clare S, Deakin LJ, Goulding D, Yen JL, Raisen C. Use of purified Clostridium difficile spores to facilitate evaluation of health care disinfection regimens. Appl Environ Microbiol 2010; 76(20):6895-900. doi: 10.1128/aem.00718-10 [Crossref] [ Google Scholar]
- Weber DJ, Rutala WA, Miller MB, Huslage K, Sickbert-Bennett E. Role of hospital surfaces in the transmission of emerging health care-associated pathogens: norovirus, Clostridium difficile, and Acinetobacter species. Am J Infect Control 2010; 38(5 Suppl 1):S25-33. doi: 10.1016/j.ajic.2010.04.196 [Crossref] [ Google Scholar]
- Schrezenmeir J, de Vrese M. Probiotics, prebiotics, and synbiotics--approaching a definition. Am J Clin Nutr 2001; 73(2 Suppl):361S-4S. doi: 10.1093/ajcn/73.2.361s [Crossref] [ Google Scholar]
- Santos VL, Nardi RM, Dias-Souza MV. Biosurfactants as Antimicrobial and Antibiofilm Agents. In: Current Developments in Biotechnology and Bioengineering. Amsterdam: Elsevier; 2017. p 371.
- Falagas ME, Rafailidis PI, Makris GC. Bacterial interference for the prevention and treatment of infections. Int J Antimicrob Agents 2008; 31(6):518-22. doi: 10.1016/j.ijantimicag.2008.01.024 [Crossref] [ Google Scholar]
- Servin AL. Antagonistic activities of lactobacilli and bifidobacteria against microbial pathogens. FEMS Microbiol Rev 2004; 28(4):405-40. doi: 10.1016/j.femsre.2004.01.003 [Crossref] [ Google Scholar]
- Singh P, Cameotra SS. Potential applications of microbial surfactants in biomedical sciences. Trends Biotechnol 2004; 22(3):142-6. doi: 10.1016/j.tibtech.2004.01.010 [Crossref] [ Google Scholar]
- Wand ME, Bock LJ, Bonney LC, Sutton JM. Mechanisms of increased resistance to chlorhexidine and cross-resistance to colistin following exposure of Klebsiella pneumoniae clinical isolates to chlorhexidine. Antimicrob Agents Chemother 2017; 61(1). doi: 10.1128/aac.01162-16 [Crossref]
- Caini S, Hajdu A, Kurcz A, Böröcz K. Hospital-acquired infections due to multidrug-resistant organisms in Hungary, 2005-2010. Euro Surveill 2013; 18(2):20352. [ Google Scholar]
- Cornejo-Juárez P, Vilar-Compte D, Pérez-Jiménez C, Ñamendys-Silva SA, Sandoval-Hernández S, Volkow-Fernández P. The impact of hospital-acquired infections with multidrug-resistant bacteria in an oncology intensive care unit. Int J Infect Dis 2015; 31:31-4. doi: 10.1016/j.ijid.2014.12.022 [Crossref] [ Google Scholar]
- Otter JA, Yezli S, Perl TM, Barbut F, French GL. The role of ‘no-touch’ automated room disinfection systems in infection prevention and control. J Hosp Infect 2013; 83(1):1-13. doi: 10.1016/j.jhin.2012.10.002 [Crossref] [ Google Scholar]
- Pettigrew MM, Johnson JK, Harris AD. The human microbiota: novel targets for hospital-acquired infections and antibiotic resistance. Ann Epidemiol 2016; 26(5):342-7. doi: 10.1016/j.annepidem.2016.02.007 [Crossref] [ Google Scholar]
- Koenigsknecht MJ, Young VB. Faecal microbiota transplantation for the treatment of recurrent Clostridium difficile infection: current promise and future needs. Curr Opin Gastroenterol 2013; 29(6):628-32. doi: 10.1097/MOG.0b013e328365d326 [Crossref] [ Google Scholar]
- Caselli E, Brusaferro S, Coccagna M, Arnoldo L, Berloco F, Antonioli P. Reducing healthcare-associated infections incidence by a probiotic-based sanitation system: a multicentre, prospective, intervention study. PLoS One 2018; 13(7):e0199616. doi: 10.1371/journal.pone.0199616 [Crossref] [ Google Scholar]
- Vandini A, Frabetti A, Antonioli P, Platano D, Branchini A, Camerada MT. Reduction of the microbiological load on hospital surfaces through probiotic-based cleaning procedures: a new strategy to control nosocomial infections. J Microbiol Exp 2014; 1(5):153-61. doi: 10.15406/jmen.2014.01.00027 [Crossref] [ Google Scholar]
- Caselli E. Hygiene: microbial strategies to reduce pathogens and drug resistance in clinical settings. Microb Biotechnol 2017; 10(5):1079-83. doi: 10.1111/1751-7915.12755 [Crossref] [ Google Scholar]
- La Fauci V, Costa GB, Anastasi F, Facciolà A, Grillo OC, Squeri R. An Innovative Approach to Hospital Sanitization Using Probiotics: In Vitro and Field Trials. J Microb Biochem Technol 2015; 7(3):160-4. doi: 10.4172/1948-5948.1000198 [Crossref] [ Google Scholar]
- Vandini A, Temmerman R, Frabetti A, Caselli E, Antonioli P, Balboni PG. Hard surface biocontrol in hospitals using microbial-based cleaning products. PLoS One 2014; 9(9):e108598. doi: 10.1371/journal.pone.0108598 [Crossref] [ Google Scholar]
- Vandini A, Frabetti A, Antonioli P, Platano D, Branchini A, Camerada MT. Reduction of the microbiological load on hospital surfaces through probiotic-based cleaning procedures: a new strategy to control nosocomial infections. J Microbiol Exp 2014; 1(5):153-61. doi: 10.15406/jmen.2014.01.00027 [Crossref] [ Google Scholar]
- Mazzacane S, Finzi G, Aparo L, Balboni PG, Vandini A, Lanzoni L. The sanitation of hospital stays: new strategies for the reduction of HAIs. Health Manage 2014; 14(3):1-12. [ Google Scholar]
- Walencka E, Rózalska S, Sadowska B, Rózalska B. The influence of Lactobacillus acidophilus-derived surfactants on staphylococcal adhesion and biofilm formation. Folia Microbiol (Praha) 2008; 53(1):61-6. doi: 10.1007/s12223-008-0009-y [Crossref] [ Google Scholar]
- Rodrigues L, van der Mei H, Banat IM, Teixeira J, Oliveira R. Inhibition of microbial adhesion to silicone rubber treated with biosurfactant from Streptococcus thermophilus A. FEMS Immunol Med Microbiol 2006; 46(1):107-12. doi: 10.1111/j.1574-695X.2005.00006.x [Crossref] [ Google Scholar]
- Rodrigues L, van der Mei H, Teixeira JA, Oliveira R. Biosurfactant from Lactococcus lactis 53 inhibits microbial adhesion on silicone rubber. Appl Microbiol Biotechnol 2004; 66(3):306-11. doi: 10.1007/s00253-004-1674-7 [Crossref] [ Google Scholar]
- Rodrigues L, van der Mei HC, Teixeira J, Oliveira R. Influence of biosurfactants from probiotic bacteria on formation of biofilms on voice prostheses. Appl Environ Microbiol 2004; 70(7):4408-10. doi: 10.1128/aem.70.7.4408-4410.2004 [Crossref] [ Google Scholar]
- van Hoogmoed CG, van der Kuijl-Booij M, van der Mei HC, Busscher HJ. Inhibition of Streptococcus mutans NS adhesion to glass with and without a salivary conditioning film by biosurfactant- releasing Streptococcus mitis strains. Appl Environ Microbiol 2000; 66(2):659-63. doi: 10.1128/aem.66.2.659-663.2000 [Crossref] [ Google Scholar]
- van der Mei HC, Free RH, Elving GJ, Van Weissenbruch R, Albers FW, Busscher HJ. Effect of probiotic bacteria on prevalence of yeasts in oropharyngeal biofilms on silicone rubber voice prostheses in vitro. J Med Microbiol 2000; 49(8):713-8. doi: 10.1099/0022-1317-49-8-713 [Crossref] [ Google Scholar]
- Al-Ghalith GA, Knights D. Bygiene: the new paradigm of bidirectional hygiene. Yale J Biol Med 2015; 88(4):359-65. [ Google Scholar]
- Burke JP. Infection control - a problem for patient safety. N Engl J Med 2003; 348(7):651-6. doi: 10.1056/NEJMhpr020557 [Crossref] [ Google Scholar]
- European Food Safety Authority (EFSA). Opinion of the Scientific Committee on a request from EFSA related to a generic approach to the safety assessment by EFSA of microorganisms used in food/feed and the production of food/feed additives. EFSA J 2005; 3(6):226. doi: 10.2903/j.efsa.2005.226 [Crossref] [ Google Scholar]
- Lebeer S, Verhoeven TL, Perea Velez M, Vanderleyden J, De Keersmaecker SC. Impact of environmental and genetic factors on biofilm formation by the probiotic strain Lactobacillus rhamnosus GG. Appl Environ Microbiol 2007; 73(21):6768-75. doi: 10.1128/aem.01393-07 [Crossref] [ Google Scholar]
- Adams MR, Marteau P. On the safety of lactic acid bacteria from food. Int J Food Microbiol 1995; 27(2-3):263-4. doi: 10.1016/0168-1605(95)00067-t [Crossref] [ Google Scholar]
- Husni RN, Gordon SM, Washington JA, Longworth DL. Lactobacillus bacteremia and endocarditis: review of 45 cases. Clin Infect Dis 1997; 25(5):1048-55. doi: 10.1086/516109 [Crossref] [ Google Scholar]
- Giamarellos-Bourboulis EJ, Bengmark S, Kanellakopoulou K, Kotzampassi K. Pro- and synbiotics to control inflammation and infection in patients with multiple injuries. J Trauma 2009; 67(4):815-21. doi: 10.1097/TA.0b013e31819d979e [Crossref] [ Google Scholar]
- Banupriya B, Biswal N, Srinivasaraghavan R, Narayanan P, Mandal J. Probiotic prophylaxis to prevent ventilator associated pneumonia (VAP) in children on mechanical ventilation: an open-label randomized controlled trial. Intensive Care Med 2015; 41(4):677-85. doi: 10.1007/s00134-015-3694-4 [Crossref] [ Google Scholar]
- Sommacal HM, Bersch VP, Vitola SP, Osvaldt AB. Perioperative synbiotics decrease postoperative complications in periampullary neoplasms: a randomized, double-blind clinical trial. Nutr Cancer 2015; 67(3):457-62. doi: 10.1080/01635581.2015.1004734 [Crossref] [ Google Scholar]